Dental Procedure Bleeding Risk Calculator
Bleeding Risk Assessment
Your Risk Assessment
Critical Instructions
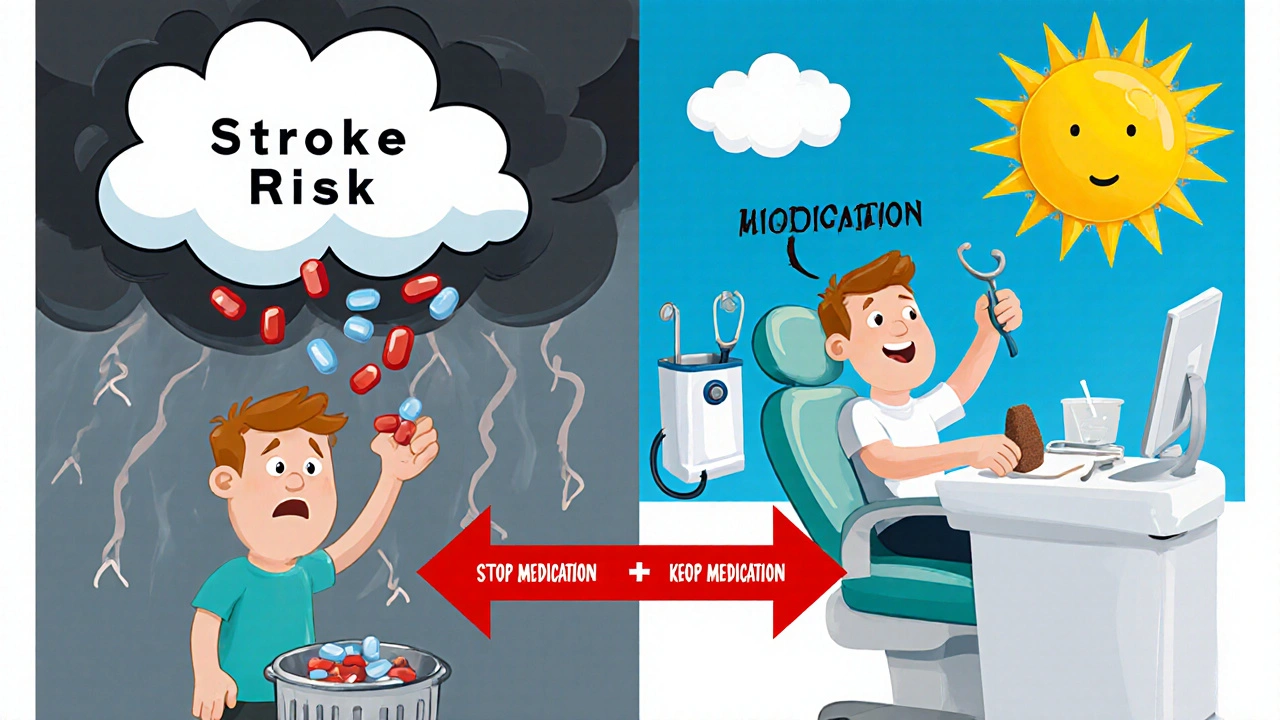
Why You Don’t Need to Stop Your Blood Thinners for Most Dental Work
It’s a common fear: you’re scheduled for a cleaning or filling, and your doctor told you to take blood thinners every day. Suddenly, you’re worried you might bleed to death at the dentist. You’re not alone. Many people assume stopping their medication is the safest move. But here’s the truth: stopping blood thinners for routine dental work is often riskier than keeping them on.
For decades, dentists and doctors would pause anticoagulants before any procedure. That changed after research showed the real danger wasn’t bleeding-it was blood clots. A single missed dose of warfarin or a DOAC can trigger a stroke, heart attack, or pulmonary embolism. The American Dental Association says this clearly now: "For most patients, it is not necessary to alter anticoagulation or antiplatelet therapy prior to dental intervention." That’s not a suggestion. It’s the standard.
Not All Dental Procedures Are Created Equal
Not every dental job carries the same bleeding risk. That’s why experts classify them into three groups:
- Low-risk: Routine cleanings, X-rays, dental impressions, and simple fillings. These cause almost no bleeding. You don’t need to do anything different.
- Low-moderate risk: Deep cleanings (scaling and root planing), root canals, crowns, and bridges. You’re still safe continuing your medication.
- Moderate risk: Removing one to three teeth, gum surgery, or removing a single impacted tooth. These require more attention, but even here, stopping your blood thinner isn’t usually needed.
The key? It’s not about the procedure-it’s about your INR level if you’re on warfarin, or the timing if you’re on a DOAC.
Warfarin and Your INR: What Numbers Matter
If you take warfarin (brand names like Coumadin or Jantoven), your doctor checks your INR-a blood test that measures how long it takes your blood to clot. For dental work:
- Low-risk procedures: INR under 3.5 is fine.
- Low-moderate risk: INR under 3.0 is ideal.
- Moderate risk: INR under 3.5 is acceptable, as long as your dentist uses extra hemostatic tools.
If your INR is above those numbers, don’t panic. Don’t skip your dose. Don’t call your dentist to cancel. Call your doctor or anticoagulation clinic first. They’ll decide if a tiny adjustment is needed-or if you’re still safe to proceed.
Studies show that even with INR levels at 4.0 or higher, most bleeding from simple extractions stops easily with pressure and special mouth rinses. The bigger risk? Letting your INR drop too low, then having a clot form while you wait for your next appointment.
DOACs: The New Normal in Blood Thinners
Today, about 60% of people starting anticoagulants get a DOAC-drugs like apixaban (Eliquis), rivaroxaban (Xarelto), or dabigatran (Pradaxa). These are easier to manage than warfarin. No regular blood tests. No food restrictions. But they still need smart timing.
For DOACs, the rule is simple: skip your morning dose on the day of a moderate-risk procedure. That’s it. No holding for days. No bridges. Just delay your pill until after your appointment.
Why? DOACs leave your system faster than warfarin. If you take your pill at 8 a.m. and have a tooth pulled at 2 p.m., there’s less than half the drug left in your blood. That’s enough to prevent clots but not enough to cause serious bleeding. Dentists in Melbourne, Sydney, and across the U.S. are now trained to ask: "When was your last dose?"-not "Are you still taking it?"

What Your Dentist Can Do to Stop the Bleeding
Your dentist isn’t just going to pull a tooth and hope for the best. They have tools designed for patients on blood thinners:
- Tranexamic acid mouthwash: A special rinse made in the pharmacy. You swish 10 mL for 1-2 minutes, then spit. Repeat every 2 hours if needed. It helps clots form faster.
- Local pressure: Gauze packed firmly over the extraction site for 30-60 minutes.
- Sutures: Stitches aren’t just for big surgery. They’re often used even for single extractions to reduce bleeding.
- Avoiding multiple extractions: If you need more than two teeth out, your dentist will space them out. No one pulls three molars in one visit if you’re on anticoagulants.
Some dentists even use fibrin sealants or oxidized cellulose (Surgicel) to pack the socket. These aren’t magic-but they work better than gauze alone.
What You Should Never Do
There are three big mistakes people make:
- Stopping your blood thinner without talking to your doctor. This is the #1 cause of preventable strokes in dental patients.
- Taking NSAIDs like ibuprofen or naproxen. These drugs make bleeding worse. Use acetaminophen (paracetamol) for pain instead.
- Ignoring post-op bleeding. A little oozing for 24 hours is normal. If you’re spitting out bright red blood every 10 minutes, or soaking through two gauze pads in an hour, call your dentist. Don’t wait until morning.
Also avoid alcohol for 48 hours after any procedure. It thins your blood further. And don’t rinse your mouth vigorously for the first 24 hours. Gentle saltwater rinses are fine after that.
Special Cases: Pregnancy, Kidney Issues, and Other Risks
Not everyone fits the standard profile. If you have:
- Chronic kidney disease
- Liver problems
- Low platelet count
- Are pregnant or postpartum
- Take aspirin or clopidogrel along with your anticoagulant
…then your risk isn’t just about the blood thinner. It’s about the whole picture. Your dentist will need to talk to your cardiologist, hematologist, or OB-GYN before proceeding.
For example, a 28-year-old woman who had a pulmonary embolism after giving birth might be on a DOAC. Her dentist will check her kidney function-because DOACs are cleared through the kidneys. If her function is low, they might delay treatment or switch to a different drug temporarily.
What to Bring to Your Appointment
Don’t wing it. Bring this to your dental visit:
- A list of all medications-including doses and times.
- Your most recent INR result (if on warfarin).
- The name and phone number of your prescribing doctor.
- Any recent lab reports showing kidney or liver function.
Many dentists now use a quick checklist before starting any procedure. If you hand them your info upfront, they can make decisions faster-and you won’t have to wait around while they call your doctor.
Bottom Line: You’re Safer With Your Blood Thinners On
Here’s the truth most people don’t hear: you’re more likely to have a stroke from skipping your blood thinner than you are to bleed dangerously from a tooth extraction.
Studies from UCSD, Stanford, and the ADA all agree: minor bleeding from dental work is manageable. Major bleeding is rare. But a clot? That can kill you in minutes.
Keep taking your medication. Tell your dentist you’re on it. Let them use the right tools. Follow their instructions. And if you’re unsure? Ask for a consultation with your doctor before your appointment. You don’t need to be afraid. You just need to be prepared.
What Happens If You Bleed After the Appointment?
It’s not common, but it can happen. Here’s what to do:
- Light oozing: Bite on a moist gauze pad for 30-45 minutes. Don’t peek. Let the clot form.
- Still bleeding: Use a damp tea bag. The tannins help clotting. Bite gently for 20 minutes.
- Heavy bleeding: Call your dentist immediately. If it’s after hours, go to the nearest emergency department. Don’t wait.
- Swelling or fever: These aren’t signs of bleeding-they’re signs of infection. Call your dentist right away.
Most patients stop bleeding within a few hours. But if you’re on a DOAC and took your pill that morning, bleeding might last a bit longer. That’s normal. Just keep pressure on it and stay calm.



Dave Pritchard
Just had a root canal last week while on Eliquis. Dentist didn’t even blink. Used that tranexamic acid rinse like they said - spit, don’t swallow. No issues. Felt fine the next day. Seriously, don’t panic. Your dentist knows what they’re doing if you give them the info upfront.