SSRI Bleeding Risk Calculator
This calculator estimates your bleeding risk based on the HAS-BLED score, which assesses factors related to bleeding risk when taking SSRIs. A score of 3 or higher indicates high risk.
Your Risk Factors
Your Results
Score indicates your bleeding risk level when taking SSRIs. Higher scores mean higher risk.
Recommended SSRI Choices
When you take an SSRI for depression or anxiety, you’re not just changing your mood-you’re also affecting how your blood clots. It’s a side effect most people never hear about until they start bruising easily or bleed longer after a cut. The truth is, SSRIs don’t just boost serotonin in your brain. They drain serotonin from your platelets, and that’s what turns a minor scrape into a problem.
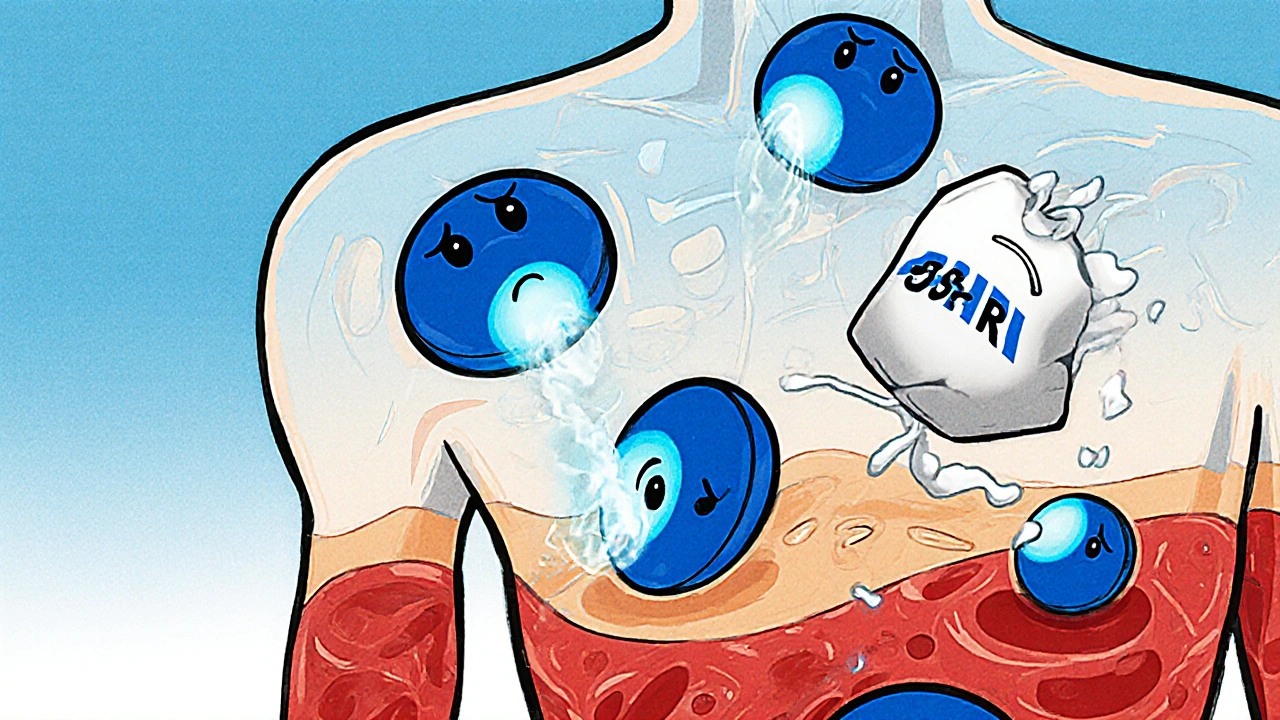
Why SSRIs Mess With Your Platelets
Platelets are the tiny blood cells that rush to a wound and stick together to stop bleeding. They need serotonin to do their job properly. About 99% of the serotonin in your blood is stored inside platelets. When you take an SSRI-like fluoxetine, sertraline, or paroxetine-it blocks the serotonin transporter (5-HTT) that normally pulls serotonin back into platelets. Without enough serotonin inside, platelets can’t activate properly. They don’t clump together as quickly or as strongly.
Studies show this isn’t theoretical. In people taking paroxetine, platelet serotonin drops by more than 80%. That’s not a small change. It’s enough to delay clot formation during injury. The effect is dose-dependent and directly tied to how tightly the drug binds to the serotonin transporter. Paroxetine and fluvoxamine bind strongest, so they cause the most platelet dysfunction. Sertraline and citalopram bind less tightly, so their impact is milder.
Not All SSRIs Are Created Equal
If you’re worried about bleeding, the SSRI you choose matters a lot. Paroxetine is the worst offender. Data from the FDA’s adverse event database shows users are 40-50% more likely to have upper GI bleeding than people on other antidepressants. Fluvoxamine isn’t far behind. Sertraline? Only a 20-30% increased risk. That’s still real-but it’s a big difference in practical terms.
Real-world reports back this up. On Reddit’s r/SSRI community, 74% of users who reported unusual bleeding were on paroxetine. Only 32% were on sertraline. Drugs.com user reviews show 18.7% of paroxetine users complained of easy bruising, compared to just 9.2% of sertraline users. This isn’t random-it’s predictable based on how the drugs interact with the serotonin transporter.
Bleeding Risk Gets Worse With Other Drugs
SSRIs alone might cause mild issues. But when combined with other medications, the risk jumps sharply. Take blood thinners like warfarin or apixaban. A 2024 JAMA Network Open meta-analysis found that people on both an SSRI and an oral anticoagulant had a 35% higher chance of major bleeding than those on anticoagulants alone. The same thing happens with NSAIDs like ibuprofen or naproxen. Together with SSRIs, NSAIDs increase bleeding risk by 4.5 times.
Even antiplatelet drugs like aspirin or clopidogrel add to the problem. But here’s the twist: a 2023 study on patients who had heart stents found that those taking SSRIs didn’t bleed more than those who didn’t-even though they were on powerful drugs like ticagrelor. Why? Because modern antiplatelet regimens are so strong that the SSRI’s effect gets drowned out. That means context matters. If you’re on multiple drugs that affect clotting, your risk is higher. If you’re only on one SSRI and otherwise healthy, your risk is low.
Who’s Most at Risk?
Not everyone on SSRIs will bleed. But some people are far more vulnerable. The HAS-BLED score helps doctors spot them. It checks for:
- Hypertension
- Abnormal kidney or liver function
- History of stroke
- Previous bleeding episodes
- Unstable blood thinners (like fluctuating INR levels)
- Age over 65
- Alcohol or drug use
If your score is 3 or higher, you’re in the high-risk group. For these people, switching from paroxetine to sertraline or citalopram can make a real difference. Sometimes, skipping SSRIs altogether and using bupropion or mirtazapine-drugs that don’t touch platelet serotonin-is the safest move.
What Happens During Surgery or Procedures?
Doctors often face a tough call: stop the SSRI and risk depression returning, or keep it and risk bleeding during surgery. For major surgeries-especially heart or brain procedures-many guidelines now say: keep the SSRI going. The risk of a depressive episode after surgery can be deadly. But for minor procedures like dental work, colonoscopies, or skin biopsies, stopping the SSRI for 5-7 days may be worth it.
There’s no one-size-fits-all rule. The American Psychiatric Association says to evaluate each case. If you’re on paroxetine and scheduled for a tooth extraction, your doctor might suggest switching to sertraline first. If you’re on sertraline and need a biopsy? Probably no change needed. Always talk to your prescriber before making any changes.
Signs You Might Be Bleeding Too Much
You don’t need to panic over every bruise. But some signs are red flags:
- Passing black, tarry stools (sign of GI bleeding)
- Vomiting blood or material that looks like coffee grounds
- Bleeding that won’t stop after 10-15 minutes of pressure
- Unexplained large bruises without injury
- Heavy menstrual bleeding that’s new or worse
- Bleeding from gums or nose with no clear cause
If you notice any of these, call your doctor immediately. Don’t wait. Early detection can prevent serious complications.
New Tools Are Helping Doctors Make Better Calls
It’s not just guesswork anymore. Electronic health records now flag when someone is prescribed an SSRI along with a blood thinner. In 2021, hospitals using Epic Systems saw a 22.4% drop in dangerous SSRI-anticoagulant combos after these alerts went live. That’s a win.
Pharmaceutical companies have updated their labels too. Paroxetine’s FDA-approved package insert now includes a boxed warning for bleeding risk in people with clotting disorders. That’s the strongest warning the FDA gives.
And now, there’s emerging science on genetics. A 2024 study found that people with the S/S version of the 5-HTTLPR gene (a serotonin transporter variant) have 2.3 times higher bleeding risk on SSRIs than those with the L/L version. Genetic testing isn’t routine yet-but it’s coming. The European Medicines Agency is reviewing whether to add genetic risk markers to SSRI labels by late 2025.
What Can You Do?
If you’re on an SSRI and worried about bleeding:
- Know your drug. Is it paroxetine or fluvoxamine? Those carry the highest risk. Sertraline or citalopram are safer bets.
- Avoid NSAIDs. No ibuprofen, naproxen, or high-dose aspirin unless your doctor says it’s okay. Use acetaminophen instead for pain.
- Watch for warning signs. Bruising, bleeding gums, dark stools-don’t ignore them.
- Talk to your doctor before any procedure. Even a simple tooth extraction might need planning.
- Don’t stop cold turkey. Stopping SSRIs suddenly can trigger withdrawal or relapse. Always taper under medical supervision.
And if you’re starting an SSRI? Ask your doctor: "Which one has the lowest bleeding risk for someone like me?" That simple question could save you from a serious complication.
It’s Not About Avoiding SSRIs-It’s About Choosing Wisely
Depression kills. Untreated, it raises your risk of heart disease, suicide, and early death. SSRIs save lives. The goal isn’t to avoid them. It’s to use them safely. For most people, the benefits far outweigh the risks. But for those with other bleeding risks-older adults, people on blood thinners, those with liver disease-the choice needs to be smarter.
The data is clear: paroxetine is the riskiest. Sertraline is the safest among SSRIs. And if you’re already bleeding or bruising easily, switching might be the best thing you do for your health. Don’t assume all antidepressants are the same. They’re not. Your platelets know the difference.
Do all SSRIs cause bleeding?
No. Not all SSRIs affect platelets the same way. Paroxetine and fluvoxamine have the strongest effect on serotonin reuptake and carry the highest bleeding risk. Sertraline and citalopram have weaker effects and are much safer for people concerned about bleeding. Fluoxetine and escitalopram fall in between.
Can I take ibuprofen with an SSRI?
It’s not recommended. Combining NSAIDs like ibuprofen or naproxen with SSRIs increases your risk of gastrointestinal bleeding by 4.5 times. Use acetaminophen (Tylenol) for pain relief instead. If you need an NSAID for a chronic condition like arthritis, talk to your doctor about alternatives or protective medications like proton pump inhibitors.
Should I stop my SSRI before surgery?
It depends. For major surgeries like heart or brain procedures, guidelines often recommend continuing SSRIs to avoid depression relapse. For minor procedures like dental work or skin biopsies, stopping the SSRI 5-7 days beforehand may reduce bleeding risk-especially if you’re on paroxetine. Always consult your doctor and surgeon together before making a decision.
Is there a blood test to check for SSRI-induced platelet dysfunction?
There isn’t a routine blood test for this. Standard coagulation tests like PT/INR or platelet count won’t show it. Specialized platelet function tests exist in research labs, but they’re not used in everyday practice. The best indicator is your clinical history: unexplained bruising, prolonged bleeding, or GI symptoms while on an SSRI.
Can genetic testing tell me if I’m at higher risk?
Yes, but it’s not standard yet. A gene variant called 5-HTTLPR affects how your body handles serotonin. People with the S/S genotype have a 2.3 times higher risk of bleeding on SSRIs than those with L/L. Testing is available through some pharmacogenomic labs and is being reviewed by European regulators for possible inclusion in drug labels by late 2025. It’s not routine, but it’s emerging as a useful tool for high-risk patients.
Are there antidepressants that don’t affect platelets?
Yes. Bupropion (Wellbutrin) and mirtazapine (Remeron) don’t block the serotonin transporter in platelets, so they don’t increase bleeding risk. They’re good alternatives for people with a history of bleeding, those on blood thinners, or older adults. They work differently than SSRIs, so they’re not a perfect replacement for everyone-but they’re safer options when bleeding risk is a concern.


Arup Kuri
so basically big pharma is just letting us bleed out while they sell us pills that make us feel better for a bit
they know this happens and still push paroxetine like its candy
its not an accident its a business model