DOAC Dose Adjustment Calculator for Kidney Disease
Calculate Your CrCl
Use Cockcroft-Gault formula: CrCl = [(140 - age) × weight (kg) × (0.85 if female)] / (72 × serum creatinine)
DOAC Dosing Recommendations
Apixaban
For patients with CrCl ≥ 15 mL/min
Use 2.5 mg twice daily if:
- Age ≥ 80 years
- Weight ≤ 60 kg
- Creatinine ≥ 1.5 mg/dL
Meet 2 or more of these criteria to use 2.5 mg dose
Rivaroxaban
Use at 20 mg once daily only if CrCl ≥ 30 mL/min
Dabigatran
Use 75 mg twice daily only if CrCl 15-30 mL/min
Edoxaban
Use 30 mg once daily if CrCl 15-50 mL/min
Why DOACs Need Special Care in Kidney Disease
Direct Oral Anticoagulants, or DOACs, are meant to be simpler than warfarin. No weekly blood tests. No strict diet rules. But if your kidneys aren’t working well, that simplicity can turn dangerous. About 1 in 3 people with atrial fibrillation also have kidney problems. And if you’re on a DOAC like apixaban, rivaroxaban, dabigatran, or edoxaban, getting the dose wrong can lead to life-threatening bleeding-or worse, a stroke because the drug isn’t working.
Unlike warfarin, DOACs leave your body mostly through your kidneys. When your kidneys slow down, the drug builds up. Too much? You bleed. Too little? You clot. It’s not guesswork. It’s math. And the math depends on one number: creatinine clearance (CrCl), not the eGFR your doctor usually sees on your lab report.
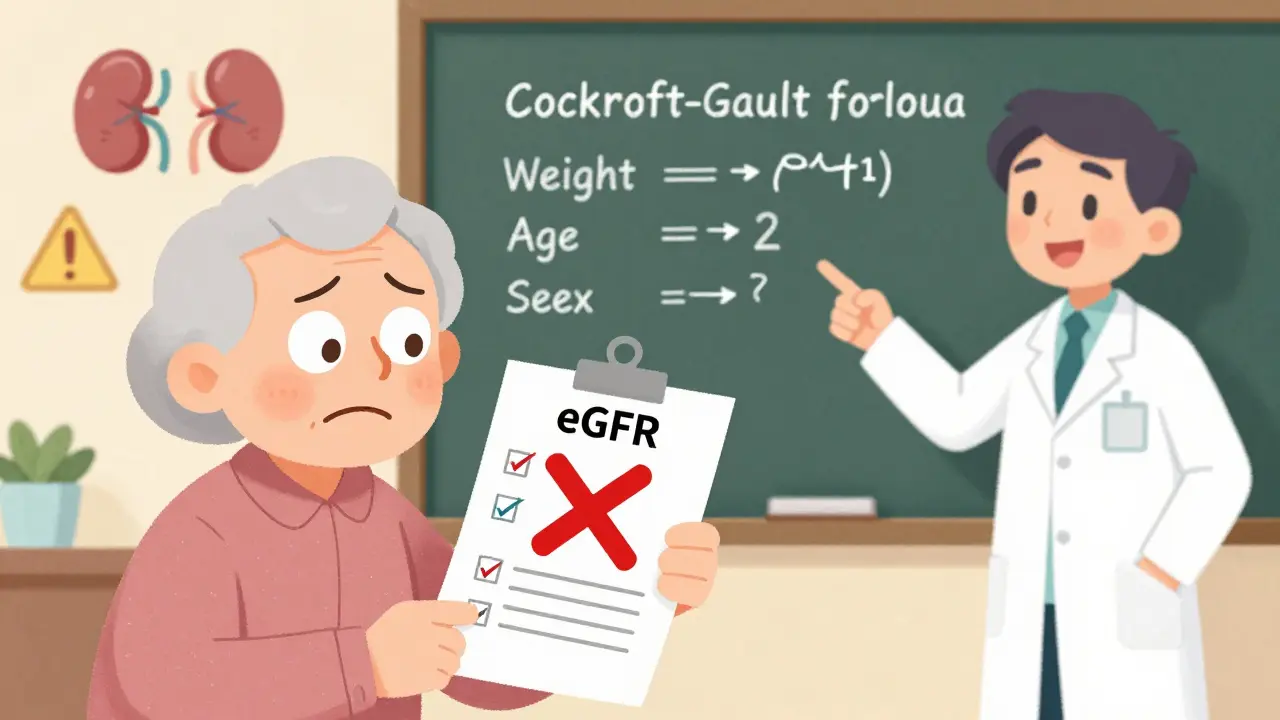
CrCl vs. eGFR: Why One Number Matters More
Most labs report eGFR-it’s easier, faster, and automated. But for DOAC dosing, eGFR is useless. The FDA, the American Heart Association, and every major guideline since 2010 say: use the Cockcroft-Gault formula. Why? Because it factors in your weight, age, and sex. eGFR doesn’t. In older, thin, or frail patients, eGFR can overestimate kidney function by 20-30%. That’s the difference between a safe dose and a deadly one.
Example: A 78-year-old woman, 52 kg, with a serum creatinine of 1.4 mg/dL. Her eGFR might read 45 mL/min. But her actual CrCl, calculated with Cockcroft-Gault, is 28 mL/min. If her doctor uses eGFR, she might get a full dose of rivaroxaban. That’s a mistake. Rivaroxaban isn’t approved below CrCl 15 mL/min. She needs a different drug or a lower dose.
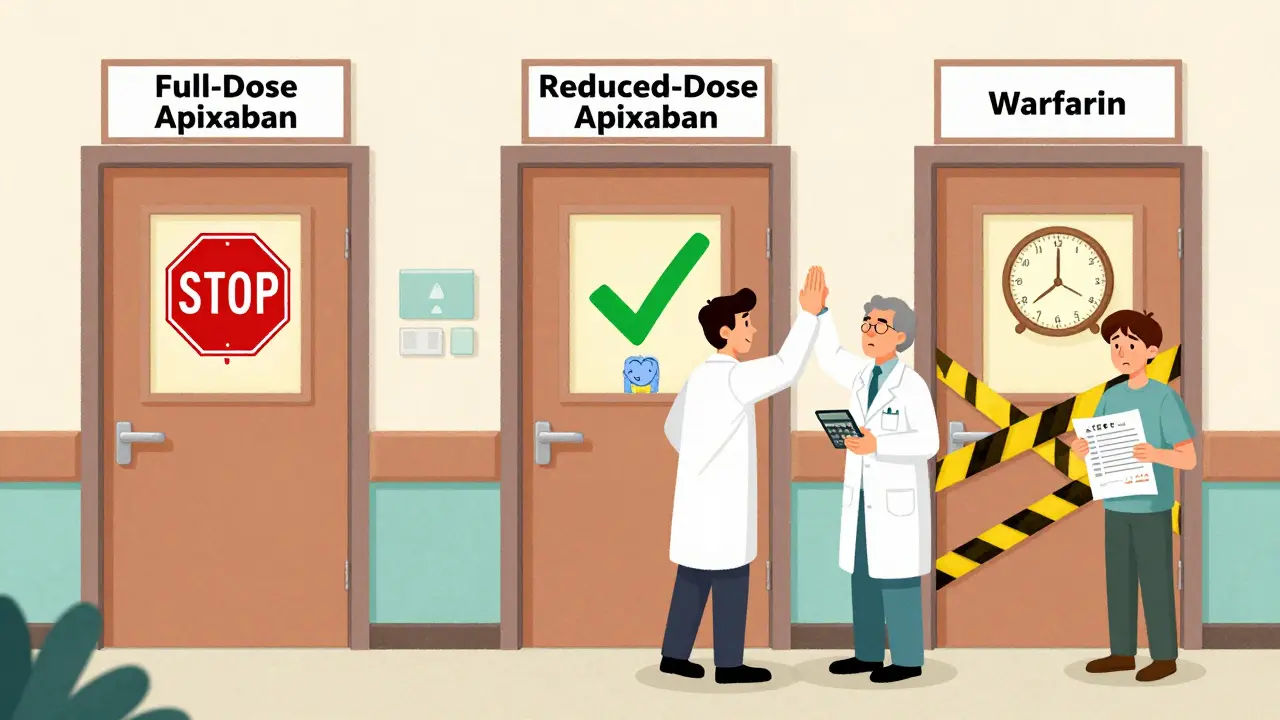
Apixaban: The Safest Choice for Kidney Problems
Among all DOACs, apixaban handles kidney impairment best. It’s the only one with data showing it’s as safe as warfarin-even in patients on dialysis. The FDA allows apixaban to be used in end-stage kidney disease, as long as the dose is cut in half. That’s 2.5 mg twice daily, not 5 mg.
You don’t need to wait for CrCl to drop to 15 before cutting the dose. You cut it if you meet two of these three criteria: you’re 80 or older, you weigh 60 kg or less, or your creatinine is 1.5 mg/dL or higher. That’s the ABC rule: Age, Body weight, Creatinine. Many doctors miss this. A 2022 JAMA study found nearly 4 in 10 DOAC prescriptions in CKD patients were wrong. Half of those were for apixaban-given at full dose when it shouldn’t have been.
Real-world data from nephrologists shows apixaban 2.5 mg twice daily cuts major bleeding by almost half compared to warfarin in dialysis patients. One clinic tracked 127 patients over 18 months. Bleeding rate: 1.8%. Warfarin group: 3.7%. That’s not a small difference. That’s life-saving.

What About the Other DOACs?
- Rivaroxaban: Avoid if CrCl is below 30 mL/min. Not approved at all below 15 mL/min. Even at 20 mL/min, the risk of bleeding jumps sharply. Many cardiologists avoid it in CKD altogether.
- Dabigatran: Only use at 75 mg twice daily if CrCl is between 15 and 30 mL/min. Anything lower? Don’t use it. It’s mostly cleared by the kidneys. Too much buildup = high bleeding risk.
- Edoxaban: Can be cut to 30 mg daily if CrCl is between 15 and 50 mL/min. Below 15? Avoid. It’s less studied in dialysis patients than apixaban.
Warfarin isn’t dead. In patients with CrCl under 15 mL/min, especially those on dialysis, warfarin is still a common choice. But it’s not better. It’s just the only one with decades of data. Studies show warfarin increases risk of intracranial bleeding and calcium buildup in blood vessels in kidney failure patients. DOACs don’t do that as much.
When to Switch or Avoid DOACs Altogether
There are red flags. If your CrCl drops below 15 mL/min, most DOACs are contraindicated. That includes dialysis patients. But apixaban is the exception. Even then, only the reduced dose is safe. Never give full-dose apixaban to someone on dialysis. I’ve seen it happen. A 79-year-old man, 58 kg, on hemodialysis. Prescribed 5 mg twice daily. He bled into his gut. Almost died.
Also avoid DOACs if you’re on dialysis and have a mechanical heart valve. No DOAC is approved for that. Warfarin is still the only option. And if you’re about to have surgery or a procedure, stop the DOAC based on your kidney function. A patient with CrCl of 25 mL/min might need to stop apixaban 48 hours before surgery. Someone with CrCl of 45 mL/min might only need to stop 24 hours before. It’s not one-size-fits-all.
How to Get the Dose Right Every Time
- Always calculate CrCl using the Cockcroft-Gault formula:
CrCl = [(140 - age) × weight (kg) × (0.85 if female)] / (72 × serum creatinine) - Double-check your inputs: Is the weight in kg? Is creatinine in mg/dL? Did you use 0.85 for women?
- Don’t rely on eGFR. Even if your EHR auto-fills it, ignore it for DOAC dosing.
- For apixaban, ask: Do I meet two of these? Age ≥80? Weight ≤60 kg? Creatinine ≥1.5 mg/dL? If yes, use 2.5 mg twice daily.
- Recheck CrCl every 3 months in CKD patients. Or sooner if they get sick, lose weight, or start new meds.
Pharmacists are your allies. Many hospitals now have anticoagulation clinics-some virtual-that track these doses. One study showed using these clinics cut adverse events by 23%. That’s 1 in 4 fewer bleeds or clots.
The Bottom Line: Simpler Isn’t Always Safer
DOACs are great-for people with normal kidneys. But kidney disease changes everything. The biggest mistake isn’t using a DOAC. It’s using the wrong dose. Apixaban at 2.5 mg twice daily is your safest bet for advanced kidney disease. Rivaroxaban? Avoid. Dabigatran? Only if CrCl is above 15. Edoxaban? Use with caution.
And always, always calculate CrCl the right way. If you’re unsure, ask a pharmacist. Or use a free online Cockcroft-Gault calculator. Don’t guess. Don’t assume. One wrong dose can kill.
What’s Coming Next?
Two big trials are wrapping up in 2025. The RENAL-AF trial is comparing apixaban to warfarin in severe kidney disease. Results will tell us if apixaban can replace warfarin even in dialysis patients. The AXIOS trial, though small, already showed apixaban levels are stable in dialysis patients-unlike other DOACs.
By 2026, we’ll likely have clearer guidelines for every stage of kidney disease. But right now? Stick to the data you have. Apixaban 2.5 mg twice daily. Avoid the others in advanced CKD. And never skip the CrCl calculation.
Can I use apixaban if I’m on dialysis?
Yes-but only at the reduced dose: 2.5 mg twice daily. This is based on FDA labeling and real-world studies showing it’s as safe as warfarin in dialysis patients. Never use the full 5 mg dose. It increases bleeding risk.
Why can’t I use eGFR to dose DOACs?
eGFR doesn’t account for body weight or sex, which affect how much drug stays in your system. In older or thin patients, eGFR overestimates kidney function. That means you might get too high a dose. Cockcroft-Gault includes weight and age, so it’s more accurate for dosing decisions.
Is rivaroxaban ever safe in kidney disease?
Only if your CrCl is above 30 mL/min. Below that, the risk of bleeding rises sharply. Rivaroxaban is not approved for use below CrCl 15 mL/min. Many doctors avoid it entirely in patients with moderate to severe kidney disease.
What’s the safest DOAC for elderly patients with kidney problems?
Apixaban, at 2.5 mg twice daily, is the safest. It’s the only DOAC with proven safety in patients over 80, with low body weight, and with CrCl as low as 15 mL/min. It’s also the only one with data in dialysis patients.
How often should kidney function be checked when on a DOAC?
At least every 3 months if you have chronic kidney disease. More often-every 1-2 months-if your kidney function is unstable, you’re over 75, or you’ve recently had a hospital stay. Changes in creatinine can happen fast, especially with dehydration or new medications.
Can I switch from warfarin to a DOAC if I have kidney disease?
Yes-if your CrCl is above 30 mL/min. For CrCl below 30, apixaban at reduced dose is the only DOAC with strong safety data. Always calculate CrCl first. Never switch blindly. Warfarin may still be safer than the wrong DOAC dose.
What to Do Next
If you’re on a DOAC and have kidney disease, ask your doctor: “What’s my CrCl? Did you use Cockcroft-Gault? Am I on the right dose?” Don’t wait for a routine visit. If your kidneys are failing, your medication needs to change. A simple calculation can prevent a trip to the ER. And if your doctor doesn’t know the answer, ask for a pharmacist to review your meds. That’s standard care now.
For those managing multiple conditions-diabetes, heart failure, high blood pressure-DOAC dosing in kidney disease is one of the most critical decisions you’ll make. Get it right. It’s not just about avoiding a clot. It’s about staying alive.


Harsh Khandelwal
So let me get this straight - we’re trusting algorithms written by Big Pharma to dose blood thinners based on a formula from 1976? 🤔 Meanwhile, the FDA’s been quietly approving DOACs like they’re energy drinks. I’ve seen three guys in my dialysis group bleed out after ‘safe’ apixaban doses. Coincidence? Or just another profit-driven checkbox? I don’t trust this. Not one bit.