When a patient switches from a brand-name drug to a generic, they often don’t realize the pills are chemically identical. But their body might react as if they’re not. That’s not because the medicine changed-it’s because their perception did.
Why Generic Medications Trigger Unexpected Side Effects
It’s not rare for someone to say, "I was fine on the brand, but since they switched me to the generic, I’ve been dizzy, tired, and anxious." The lab reports show the same active ingredient, same dose, same absorption rate. So what’s going on?
The answer lies in the nocebo effect-a psychological phenomenon where negative expectations cause real, physical symptoms. The word comes from Latin: nocebo means "I shall harm." Unlike the placebo effect, where hope improves outcomes, the nocebo effect turns fear into pain, fatigue, nausea, or headaches-even when the drug has no active component.
A 2025 study tested this with sham oxytocin sprays. Healthy volunteers were told they were getting either a branded version (simple name, high price) or a generic (complex name, low price). Both sprays were sugar water. Yet those told they were using the generic reported significantly more side effects. Their bodies reacted to the label, not the liquid.
This isn’t just a lab quirk. In the U.S., 90% of prescriptions are for generics, but nearly 4 in 10 patients still believe generics are less effective. And when they believe that, their bodies often prove them right-even when they’re wrong.
How Packaging and Price Shape Your Experience
It’s not just the name on the bottle. The box, the color, the font, even the weight of the pill can trigger the nocebo effect.
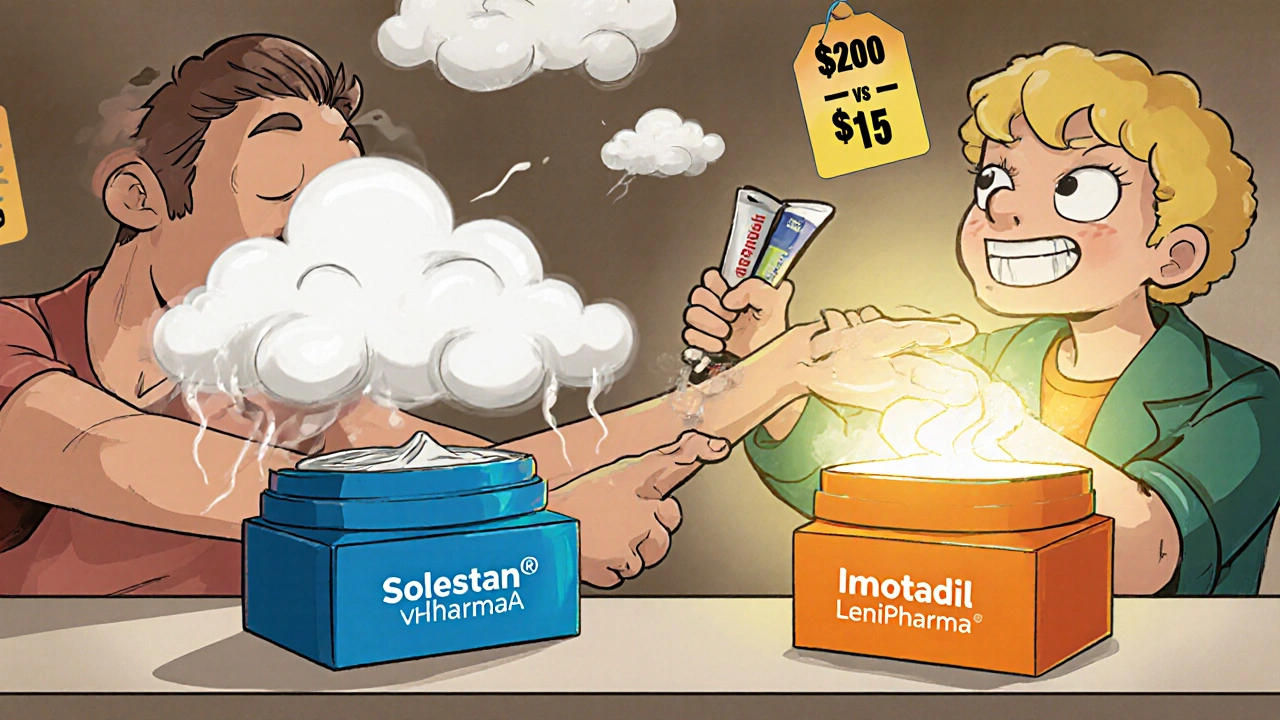
In one experiment, researchers gave people an inert cream labeled either "Solestan® Creme" in a sleek blue box or "Imotadil-LeniPharma Creme" in a plain orange container. Both had zero active ingredients. But those using the "expensive" cream reported more pain sensitivity-because they expected to.
It’s the same with pills. A generic version of a brand-name antidepressant might look different: smaller, white, with a weird letter-number code. Patients who’ve been on the original for years see that change and think: This isn’t the same. It’s cheaper. It must be weaker. Their brain starts scanning for symptoms. A normal headache? Must be the pill. A bad night’s sleep? The generic’s fault.
And it’s not just patients. Doctors, pharmacists, and even online forums reinforce the idea. Reddit threads like "My sertraline generic made me feel awful" get thousands of upvotes. No one says, "My brand-name version made me feel awful, but the generic didn’t." The narrative is one-sided-and it sticks.
What Bioequivalence Really Means
The FDA and other global regulators don’t just approve generics because they’re cheaper. They require proof that the generic delivers the same amount of active ingredient into the bloodstream at the same speed as the brand. That’s called bioequivalence.
To qualify, the generic’s absorption rate (AUC) and peak concentration (Cmax) must fall within 80-125% of the brand’s. That’s a tight range-tighter than the variation you’d see between two batches of the same brand-name drug.
Yet patients assume the generic is "less precise." They don’t realize that brand-name drugs themselves vary between batches. One bottle of Prozac might be 98% of the target concentration. Another might be 102%. The generic? Same thing. But because it’s labeled "generic," the brain treats it like a mistake.
Even "authorized generics"-the exact same pills made by the brand-name company but sold under a generic label-still trigger nocebo effects. In one 2023 study, patients switched from a brand to its own authorized generic reported more side effects. The drug didn’t change. Only the label did.
How Healthcare Providers Can Reduce the Nocebo Effect
It’s not enough to say, "It’s the same medicine." That’s what most providers do-and it often backfires.
Here’s what works:
- Reframe the message. Instead of saying, "We’re switching you because it’s cheaper," say, "This medication has the exact same active ingredient as your previous one, and studies show patients do just as well-or better-on it. Many people actually feel more stable once they switch."
- Avoid listing every possible side effect. Saying, "This drug can cause nausea, dizziness, headache, insomnia, weight gain, and mood swings" primes the brain to look for those symptoms. Say instead, "Most people tolerate this well. If you notice any changes, we’ll work together to figure out what’s happening."
- Use authority with care. Patients trust their doctor. If you say, "This is a good option," they’re more likely to believe it. But if you say it like you’re rushing, or like you’re just cutting costs, they’ll hear skepticism.
- Explain the cost savings. A 2022 study found that when patients learned switching to a generic could save them over $3,000 a year, nocebo effects dropped by 37%. Money matters-but not just because it’s cheaper. It shows you’re looking out for their whole life, not just their prescription.
Kaiser Permanente uses a script for these conversations: "This medication contains the exact same active ingredient as what you were taking before. Studies show patients do just as well on the generic version. If you notice anything different, we’ll adjust it together."
That script works because it’s honest, positive, and collaborative.
When Patients Already Feel Worse After Switching
What if a patient comes in already convinced the generic is making them sick? They’ve read the forums. They’ve talked to friends. They’re convinced.
Don’t dismiss them. Don’t say, "It’s all in your head." That shuts down trust.
Instead:
- Ask: "What’s different since you switched?" Let them describe it in their own words.
- Validate: "It makes sense you’d feel that way. Lots of people worry about this when they switch."
- Explain: "Your body is extra alert right now because you’re expecting side effects. That can make normal sensations feel stronger."
- Test: If symptoms are mild and not dangerous, suggest staying on the generic for 2-4 weeks. Often, the brain recalibrates. Symptoms fade.
- Offer alternatives: If symptoms persist and are severe, consider switching back-then document why. Sometimes, the psychological burden outweighs the cost savings.
There’s no shame in going back to the brand if it’s what the patient needs to feel stable. The goal isn’t to force generics-it’s to make sure patients feel safe, heard, and supported.

Long-Term Solutions: Changing the Culture Around Generics
One-off conversations won’t fix this. The nocebo effect is a cultural problem.
Pharmacies can help by using neutral packaging-not mimicking brands, but not making generics look "cheap" either. The European Medicines Agency recommends this balance: avoid confusion, but avoid alarm.
Public health campaigns need to show real data: "9 out of 10 prescriptions in the U.S. are generics. 9 out of 10 patients get the same results."
And we need to stop letting pharmaceutical marketing shape perception. Brand-name ads paint their drugs as premium. Generic ads? Rarely exist. That silence says: "This isn’t worth talking about." But it’s worth talking about-because millions of people rely on it.
Some companies now use "branded generics"-same pills, same packaging style as the original. It’s not deceptive. It’s just smart design. If the box looks familiar, the brain doesn’t panic.
Final Thought: It’s Not About the Pill. It’s About the Story
The pill doesn’t change. The body doesn’t change. What changes is the story the patient tells themselves.
When they hear "generic," they hear "inferior." When they see a different color, they hear "something’s wrong." When they save money, they think, "I got the cheap version. That’s why I feel awful."
That story isn’t true. But it feels true.
Our job isn’t to argue with the story. It’s to rewrite it-with facts, with empathy, and with consistency. Because the medicine works. But the mind decides whether the patient believes it does.
Do generic medications have the same active ingredients as brand-name drugs?
Yes. By law, generic medications must contain the exact same active ingredient, strength, dosage form, and route of administration as the brand-name version. Regulatory agencies like the FDA and EMA require proof that the generic delivers the same amount of medicine into the bloodstream at the same rate-within a strict 80-125% range. This is called bioequivalence. The only differences are in inactive ingredients like fillers, dyes, or packaging.
Why do some people feel worse on generic medications?
It’s usually not because the medicine is different-it’s because of the nocebo effect. When patients expect side effects-because the pill looks different, costs less, or they’ve heard stories from others-their brain becomes hyper-aware of normal bodily sensations. A slight headache or tiredness gets labeled as a side effect. Studies show this happens even with identical drugs, like authorized generics made by the same company as the brand. Perception drives the experience.
Can packaging and labeling influence side effects?
Yes. Research shows that packaging design, color, and price cues can trigger stronger side effect reports-even with inert substances. In one study, people using a cream in a sleek, expensive-looking box reported more pain sensitivity than those using the same cream in a plain generic-looking package. The same applies to pills: a white, unbranded tablet can feel "less trustworthy" to someone used to a colorful brand-name pill, leading to increased anxiety and symptom reporting.
Should I switch back to the brand if I feel worse on the generic?
It depends. If symptoms are mild and started right after switching, try staying on the generic for 2-4 weeks. The brain often adjusts. But if symptoms are severe, persistent, or affecting your quality of life, switching back is reasonable. Your comfort and mental health matter as much as cost savings. Talk to your provider about your experience-they can help you decide whether to stay on the generic, try another, or return to the brand.
Are generic medications less regulated than brand-name ones?
No. Generic medications undergo the same rigorous testing as brand-name drugs. They must meet the same quality, safety, and effectiveness standards. In fact, many generics are made in the same factories as brand-name drugs. The FDA inspects both types equally. The difference isn’t in regulation-it’s in perception.
How can I reduce my own nocebo effect when taking generics?
Start by learning the facts: generics are proven to work the same. Avoid online forums that focus only on negative experiences. When you get your prescription, ask your pharmacist: "Is this the same medicine as before?" If yes, remind yourself: "This is the same drug. My body just needs time to adjust to the new look." If you notice symptoms, track them objectively-don’t assume every change is the pill’s fault. And if you’re still worried, talk to your doctor. Knowledge reduces fear.



Arpita Shukla
Interesting how the brain tricks you. I work in pharma QA in India, and I've seen generics made in the same facility as brands. Same machines, same batch logs. The only difference? The sticker on the bottle. Patients swear the generic made them sick-yet their blood levels show identical absorption. It’s not the drug. It’s the story they tell themselves.