One wrong letter on a prescription can kill someone. It’s not science fiction. It’s happened-again and again. A doctor writes "MS" for morphine sulfate. The pharmacist reads it as magnesium sulfate. A patient gets the wrong drug. They go into cardiac arrest. They don’t wake up. This isn’t rare. It’s predictable. And it’s preventable.
Why These Abbreviations Are Deadly
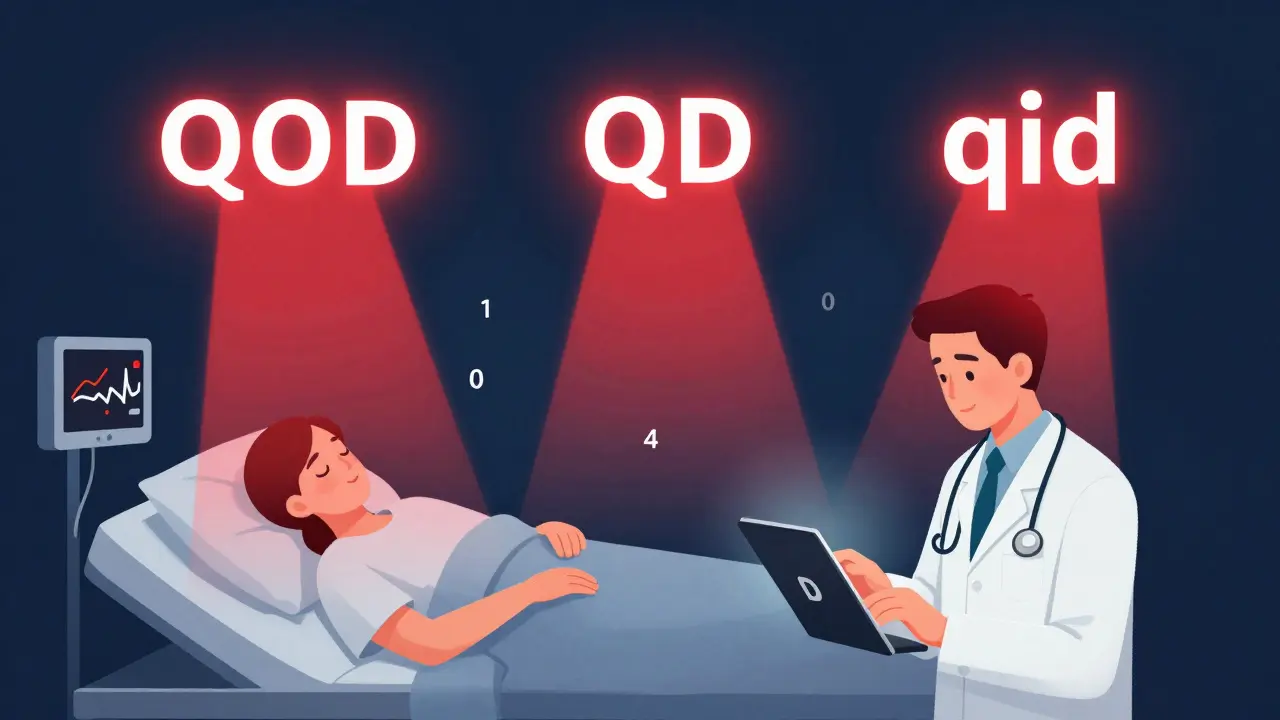
The problem isn’t that doctors are careless. It’s that some abbreviations look too similar, sound too alike, or mean different things depending on who’s reading them. The Joint Commission and the Institute for Safe Medication Practices (ISMP) have been warning about this for over 20 years. Their "Do Not Use" list isn’t a suggestion. It’s a safety rule. And ignoring it puts lives at risk.The most dangerous abbreviation? "QD"-meant to mean "once daily." But when handwritten, it looks like "QOD" (every other day) or even "qid" (four times daily). In a 2018 analysis of nearly 5,000 medication errors, "QD" was involved in 43.1% of all abbreviation-related mistakes. A patient meant to get one dose a day got four. That’s a toxic overdose.
Then there’s "U" for units. It looks like a zero, a four, or even "cc" (cubic centimeters). A diabetic patient was given 100 U of insulin instead of 10 U because the "U" was misread as "10." That’s a lethal dose. Another case: "IU" for international unit was mistaken for "IV" (intravenous), leading to a drug being injected directly into a vein when it was meant to be given slowly under the skin.
And "cc"? It’s been banned for years. But you still see it. It’s confused with "u" (units) or "mL" (milliliters). One pharmacist intercepted an order for "5 cc" of a concentrated solution-thinking it was 5 mL. It was actually 5 units of a drug that should’ve been given in micrograms. The patient could’ve died.
The Drug Abbreviation Trap
Some abbreviations are worse because they sound like other drugs. "MS" or "MSO4" for morphine sulfate? It’s a nightmare. Magnesium sulfate is written as "MgSO4." One letter difference. One letter misread. One patient dead."AZT" for zidovudine (an HIV drug) has been mistaken for azathioprine (an immune suppressant) or aztreonam (an antibiotic). The wrong drug means the patient’s condition gets worse-or they develop dangerous side effects from a drug they shouldn’t have.
"TAC" for triamcinolone cream? Sounds like "Tazorac," a completely different acne medication. A patient with eczema got Tazorac instead. It burned their skin. They needed emergency treatment.
"DTO" for diluted tincture of opium? Sounds like morphine sulfate. One pharmacy chain reported five near-misses in a single year because of this one abbreviation.
"BIW" (twice weekly) was misread as "twice daily" in a case involving chlorambucil, a chemotherapy drug. The patient received double the intended dose. They developed severe bone marrow suppression. They spent weeks in the hospital.
What’s on the Official "Do Not Use" List
The Joint Commission’s official list is short but deadly serious. Here are the top ones you must never use:- QD - Use "daily" instead
- QOD - Use "every other day"
- QHS - Use "at bedtime"
- BIW - Use "twice weekly"
- U - Use "unit"
- IU - Use "international unit"
- MS or MSO4 - Use "morphine sulfate"
- MgSO4 - Never abbreviate; write it out
- cc - Use "mL"
- SC or SQ - Use "subcutaneous"
- NMT - Avoid entirely; describe the treatment
- TAC - Write out "triamcinolone"
That’s 12 items. But ISMP’s full list has 127. Why? Because in community pharmacies, long-term care, and outpatient clinics, even more abbreviations sneak in. "DOR," "TAF," and "TDF"-abbreviations for antiretroviral drugs-were added to the list in January 2024 after a 227% spike in errors from 2019 to 2023.
How Technology Helps-And Fails
Electronic health records (EHRs) were supposed to fix this. And they did-mostly. A 2021 study found EHRs cut abbreviation errors by 68%. But 12.7% of errors still happened. Why? Because doctors still type free-text notes. "Give MS 10 mg SC." The system doesn’t always flag it. Or worse-it auto-fills a wrong abbreviation because it’s seen it before.Some hospitals now use AI tools that scan every order in real time. Epic Systems rolled this out to 72% of U.S. hospitals by late 2023. It flags "QD," "U," "MS," and others before the prescription leaves the computer. But not all systems have it. And if you’re a private practice doctor using paper or an old EHR? You’re still on your own.
Why People Still Use Them
You’d think after 20 years of warnings, everyone would stop. But they don’t. A 2022 survey by the American Medical Association found 43.7% of physicians over 50 still use banned abbreviations. They learned them in medical school in the 1980s. "It’s faster," they say. "We’ve always done it this way."It’s not laziness. It’s habit. And habits die hard. One nurse told a story: she caught a "U" on a prescription and corrected it. The doctor wrote back: "I’ve been writing U for 30 years. You’re making me look bad."
Change is slow. But the cost of not changing? It’s measured in lives.
What Works: Real Solutions
The best programs don’t just ban abbreviations. They build systems around safety.Mayo Clinic did it right. They:
- Blocked all banned abbreviations in their EHR with hard stops-you can’t submit the order unless you fix it
- Trained every prescriber, nurse, and pharmacist in a mandatory 90-minute session
- Added real-time alerts when someone typed "QD" or "U"
- Published monthly reports showing how many errors were caught
Result? A 92.3% drop in abbreviation-related errors in 18 months.
Another trick: write out the drug name, the dose, and the route in full. "Morphine sulfate 10 mg subcutaneous daily." No abbreviations. No guessing. No risk.
What Happens When You Ignore This
The Joint Commission can shut down a hospital for not following this rule. It’s part of their accreditation standards. CMS can cut Medicare reimbursements by up to 1% for hospitals with too many abbreviation-related errors. But the real penalty? The patient who dies because someone wrote "MS" instead of "morphine sulfate."Pharmacists are the last line of defense. A 2022 ASHP survey found 63.7% of pharmacists intercepted at least one dangerous abbreviation error in the past year. The top three? "QD," "U," and "MS." That’s not luck. That’s vigilance.
But you shouldn’t need a pharmacist to save someone from a doctor’s bad handwriting.
What You Can Do
If you’re a patient: ask. "Is this morphine sulfate? Or magnesium sulfate?" Read your prescription. If you see "U," "QD," or "MS," ask for it to be written out.If you’re a provider: stop using them. Even if you’ve used them for decades. Your patient doesn’t care about your habits. They care about living.
If you’re a pharmacist: don’t guess. Call the prescriber. Even if it’s 2 a.m. One call can save a life.
There’s no excuse anymore. We have the tools. We have the data. We have the rules. The only thing missing is consistency.
Stop abbreviating. Start writing. Lives depend on it.
What’s the most dangerous medical abbreviation?
The most dangerous abbreviation is "QD" (once daily), which was involved in 43.1% of all abbreviation-related medication errors in a 2018 ISMP analysis. It’s often misread as "QOD" (every other day) or "qid" (four times daily), leading to dangerous overdoses. "U" for units and "MS" for morphine sulfate are also top killers, frequently mistaken for zero, four, or magnesium sulfate.
Why can’t doctors just write "daily" instead of "QD"?
They can-and they should. "Daily" is clearer, faster to read, and impossible to misinterpret. Some doctors resist because they learned "QD" in medical school decades ago. But speed isn’t worth safety. Writing out "daily" takes the same amount of time as typing "QD," and it eliminates confusion. Electronic systems now auto-correct "QD" to "daily," making it even easier.
Are electronic health records enough to prevent these errors?
No. While EHRs reduced abbreviation errors by 68%, 12.7% of errors still happen because doctors use free-text fields or override safety alerts. Systems that block banned abbreviations with hard stops (not just warnings) cut errors by 84.6%. Without enforcement, technology alone won’t save lives.
What should I do if I see "U" on a prescription?
Never assume. Call the prescriber and confirm it means "unit." Then, insist it be written out as "unit" on the label. "U" has been mistaken for "0," "4," or "cc"-all of which can cause fatal overdoses. Pharmacists intercepted "U" errors in nearly 29% of cases in 2022. Don’t rely on someone else to catch it.
Is this a problem only in the U.S.?
No. Canada, the UK, Australia, and other countries have similar "Do Not Use" lists. The ISMP Canada list includes additional entries for community pharmacies. The problem exists wherever handwritten or poorly structured prescriptions are used. Even in high-tech hospitals, if staff aren’t trained, the risk remains.
How can I tell if my doctor is using dangerous abbreviations?
Look for single letters or unclear terms: "QD," "U," "MS," "cc," "BIW," or "TAC." If you see them, ask: "Can you write that out?" A good doctor won’t mind. A bad one will get defensive. Your safety matters more than their convenience. If your prescription looks like a code, it’s not normal-it’s risky.



Teresa Marzo Lostalé
Man, I read this and just felt my chest tighten. Like, we’re talking about people dying because someone typed "U" instead of "unit"? That’s not a mistake - that’s a system failure. And yet we still act like it’s just "how things are done."
I work in a clinic, and I’ve seen nurses double-checking scripts like they’re decoding ancient runes. It’s exhausting. And sad. We’ve got tech that could fix this - but we’d rather keep clinging to our old habits like they’re family heirlooms.
It’s not laziness. It’s grief. We’re mourning the slow death of care in medicine. And no one wants to admit it.