More than 1 in 3 adults over 60 are taking five or more prescription drugs. That’s not just common-it’s dangerous. Every extra pill adds risk. Not because the drugs themselves are bad, but because polypharmacy turns simple treatments into ticking time bombs. A blood pressure med here, a sleep aid there, an OTC painkiller on top-it all adds up. And when these pills interact, the results aren’t just uncomfortable. They’re life-threatening.
What Exactly Is Polypharmacy?
Polypharmacy isn’t just having a lot of meds. It’s taking five or more medications regularly, especially when some aren’t truly needed. The CDC says 33% of Americans in their 60s and 70s are in this zone. And it’s not just older adults. People with chronic conditions-diabetes, heart disease, arthritis-are often caught in the same trap. Each new drug is prescribed to fix a problem caused by another. That’s called a prescribing cascade. For example: an opioid causes constipation, so a laxative is added. Then the laxative causes electrolyte imbalance, so another drug is prescribed to fix that. Suddenly, someone’s on 12 pills just to manage side effects of the first three.The Most Dangerous Combinations You Need to Know
Not all drug combos are equal. Some are quietly deadly. Here are the top high-risk pairs and trios that show up again and again in emergency rooms and hospital admissions:- Warfarin + cranberry juice: Warfarin thins your blood. Cranberry juice makes it thinner-way too thin. This combo has sent people to the ER with internal bleeding.
- Statins + grapefruit juice: Grapefruit blocks the enzyme that breaks down statins. That means too much drug builds up in your body, leading to rhabdomyolysis-a condition where muscle tissue breaks down and can kill your kidneys.
- BP meds + decongestants (like pseudoephedrine): Decongestants spike blood pressure. If you’re already on lisinopril or metoprolol, this combo can trigger a stroke or heart attack.
- Acetaminophen + oxycodone + prochlorperazine: This trio shows up in nearly 30% of ER visits among seniors in the 30 days before admission. Why? Sedation piles on sedation. Dizziness turns to falls. Falls turn to broken hips.
- Benzodiazepines (like diazepam) + opioids: Both depress breathing. Together, they’re a leading cause of accidental overdose in older adults.
And it’s not just prescriptions. Over-the-counter meds and supplements make up 40% of the dangerous combos found in cancer patients alone. Antacids, herbal sleep aids, fish oil, even vitamin E can interfere with how your body handles meds.
The Beers Criteria: Your Go-To Risk Filter
The American Geriatrics Society updated the Beers Criteria in 2019 for a reason: it’s the most trusted tool doctors and pharmacists use to spot risky drugs in older adults. It flags medications that should be avoided-or used with extreme caution-in people over 65. Here’s what it says to watch for:- Anticholinergics: Drugs like diphenhydramine (Benadryl), oxybutynin, and even some antidepressants. They cause confusion, dry mouth, urinary retention, and worsen dementia.
- Benzodiazepines: Even short-term use increases fall risk by 50%. Long-term? Higher chance of addiction and memory loss.
- α1-blockers (like doxazosin): Used for prostate or high blood pressure, but they cause sudden drops in blood pressure when standing. That’s how people end up in the ER after a fall.
- NSAIDs (like ibuprofen): Dangerous for those with kidney disease, heart failure, or on blood thinners. They can cause internal bleeding and acute kidney injury.
If you’re on any of these, ask: Is this still necessary? Often, the answer is no.
How to Build Your Own Polypharmacy Risk Checklist
You don’t need a doctor to start. Here’s how to take control:- Make a full list. Write down every pill, patch, liquid, supplement, and OTC med you take-even the ones you only use once a week. Include brand names and doses.
- Bring it to every appointment. Don’t rely on memory. Don’t assume your doctor knows what you’re taking. Hand them the list.
- Ask three questions:
- Why am I taking this?
- What happens if I stop it?
- Could this interact with anything else I’m on?
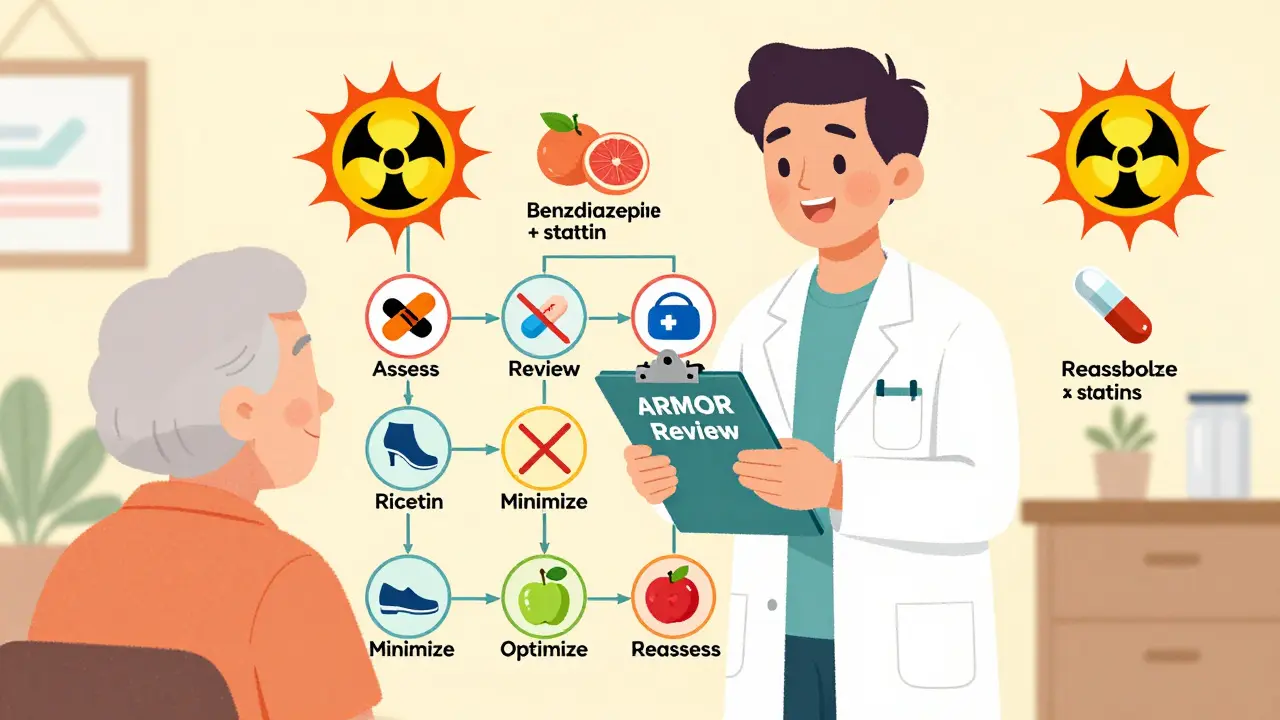
- Use the ARMOR tool:
- Assess: What’s the purpose of each med?
- Review: Check for Beers Criteria flags and known interactions.
- Minimize: Can any be stopped or lowered?
- Optimize: Are there safer alternatives?
- Reassess: Revisit every 3-6 months or after any hospital visit.
- Get a pharmacist involved. Pharmacists are trained to catch interactions doctors miss. Ask for a free med review at your pharmacy.
Real People, Real Consequences
A 72-year-old woman in Ohio was on 11 medications. She started feeling dizzy, confused, and fell twice. Her daughter brought her list to a pharmacist. The pharmacist spotted three drugs on the Beers Criteria list, plus a dangerous combo: a sleep med and a painkiller that both caused sedation. Within two weeks, two meds were stopped. Within a month, her dizziness was gone. She went from 11 pills to 6.Another man in Florida took statins, a blood thinner, and a daily antacid. He started having muscle pain and dark urine. His doctor blamed aging. He didn’t mention the antacid. Turns out, the antacid blocked his statin’s metabolism. His kidneys were under stress. He was hospitalized for rhabdomyolysis. He didn’t know antacids could do that.
These aren’t rare cases. A 2020 study of 59 seniors found 70% were at risk of dangerous interactions. And 67% were taking at least one medication the Beers Criteria says should be avoided.
What’s Being Done? And What’s Not Working
Hospitals and clinics use electronic alerts to warn doctors about bad combos. But here’s the problem: 96% of these alerts get ignored. Why? Alert fatigue. If your computer beeps every 3 minutes about something you’ve seen a hundred times, you stop listening.That’s why tools like ARMOR and pharmacist-led reviews are more effective than tech alone. The World Health Organization now calls polypharmacy a global safety crisis. Their 2023 initiative aims to cut severe harm from meds by 50% by 2027. But that won’t happen unless patients and families speak up.
What You Can Do Today
You don’t have to wait for your next appointment. Start now:- Write down every medication you take. Include supplements and OTCs.
- Look up each one on the Beers Criteria list (search “American Geriatrics Society Beers Criteria 2019”).
- Check for grapefruit, cranberry, or alcohol interactions.
- Call your pharmacy and ask for a free medication review.
- Bring your list to your next doctor visit. Say: “I want to make sure I’m not on anything dangerous.”
Medications save lives. But too many at once can end them. The goal isn’t to stop all your meds. It’s to stop the ones that don’t belong. One less pill can mean one less fall, one less ER visit, one more year at home.
What is the most common dangerous drug combination in older adults?
The most common dangerous combo involves blood pressure medications paired with over-the-counter decongestants like pseudoephedrine. This can cause sudden, severe spikes in blood pressure, increasing stroke risk. Another top risk is combining benzodiazepines (sleep or anxiety meds) with opioids, which can dangerously slow breathing. Both are frequently overlooked because one drug is prescribed and the other is bought without a prescription.
Can over-the-counter meds really cause serious interactions?
Absolutely. About 40% of dangerous drug interactions in older adults involve OTC meds or supplements. Common culprits include antacids (like Tums or Pepcid), sleep aids (like Unisom or Benadryl), pain relievers (like ibuprofen), and herbal products like St. John’s Wort or garlic supplements. These can interfere with blood thinners, antidepressants, statins, and even chemotherapy drugs. Just because it’s sold on a shelf doesn’t mean it’s safe with your prescription meds.
How often should I review my medications?
You should review your meds every 3 to 6 months-or anytime you start, stop, or change a medication. After a hospital stay, emergency room visit, or major illness, do a full review immediately. Many people don’t realize their list grows over time. A simple check-up can uncover pills you’ve been taking for years with no clear reason.
Is polypharmacy always bad?
No. For someone with heart failure, diabetes, and kidney disease, multiple medications may be necessary and life-saving. The problem isn’t the number of pills-it’s whether each one is still needed, effective, and safe with the others. Polypharmacy becomes dangerous when it’s unmanaged, unreviewed, or driven by habit instead of medical need.
What’s the ARMOR tool and how do I use it?
ARMOR is a five-step process designed by pharmacists to safely reduce unnecessary medications: Assess (why is each drug prescribed?), Review (check for Beers Criteria flags and interactions), Minimize (can any be stopped?), Optimize (are there safer alternatives?), and Reassess (check progress every few months). You can use it yourself by making a list and asking your pharmacist or doctor to walk through each step with you. Many clinics now use this exact method during medication reviews.
Can I just stop a medication if I think it’s causing problems?
Never stop a prescription drug suddenly without talking to your doctor. Some meds-like blood pressure pills, antidepressants, or steroids-can cause dangerous withdrawal effects if stopped abruptly. Instead, make a list of your symptoms and bring them to your provider. Ask: “Could this be from one of my meds? Can we try lowering the dose or stopping it safely?” Most doctors will agree to a trial discontinuation if it’s done carefully.



Siobhan K.
This is the kind of post that should be mandatory reading for every geriatric patient and their family. The Beers Criteria isn't just a checklist-it's a lifeline. I've seen too many seniors on 12 meds just because no one ever asked if they still needed them. Pharmacists are the unsung heroes here.