When you pick up a generic pill from the pharmacy, you expect it to work just like the brand-name version. You’re not just saving money-you’re trusting that the science behind it is solid. But how do we know it’s truly the same? That’s where bioequivalence comes in. It’s not marketing. It’s not guesswork. It’s a rigorous, science-based process that decides whether a generic drug can safely replace the original. And if this testing fails, patients could be at risk.
What Bioequivalence Really Means
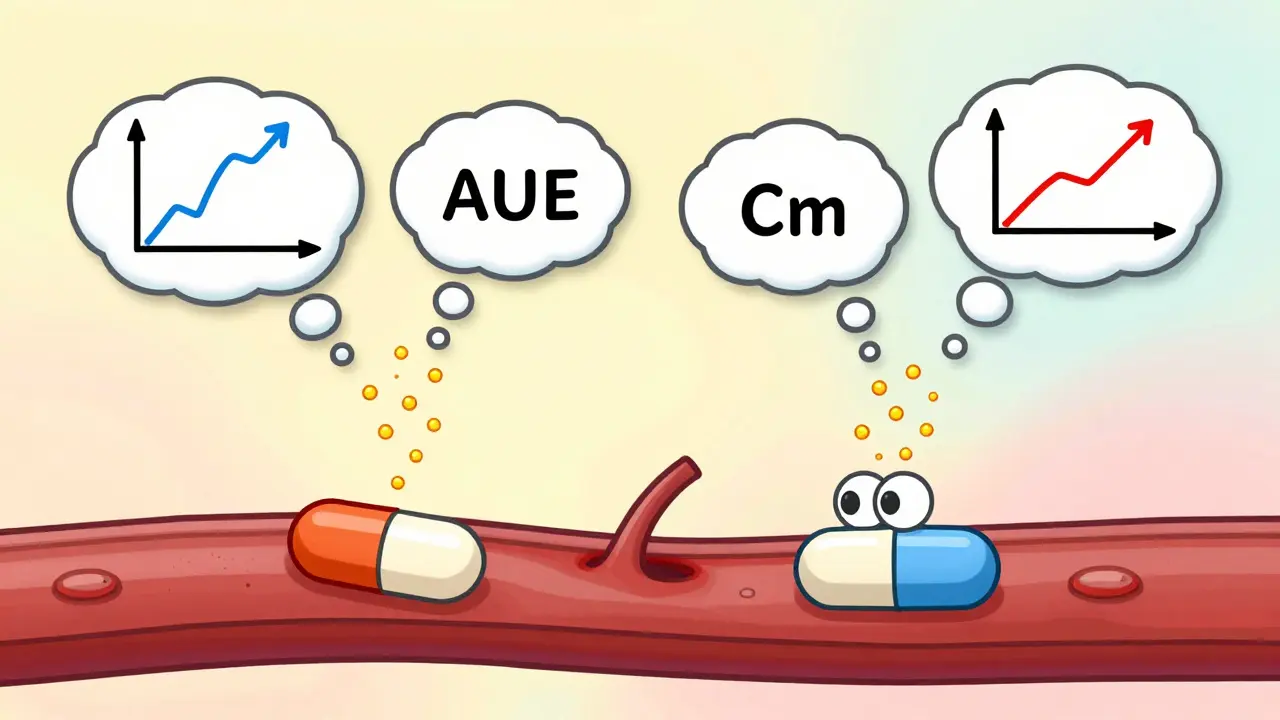
Bioequivalence isn’t about matching ingredients. It’s about matching what happens inside your body. Two drugs are bioequivalent if they deliver the same amount of active ingredient to your bloodstream at the same rate. That means your body absorbs and uses them in nearly identical ways. This isn’t theoretical-it’s measured using real data from blood tests. The key numbers are AUC (how much drug gets into your system over time) and Cmax (how high the drug peaks in your blood).The global standard? The 90% confidence interval for both AUC and Cmax must fall between 80% and 125% compared to the brand-name drug. That’s not arbitrary. It’s based on decades of clinical data showing that within this range, there’s no meaningful difference in how the drug works or how safe it is. For most drugs, this gap is wide enough to account for normal biological variation between people-but tight enough to prevent dangerous shifts.
Take warfarin, for example. It’s a blood thinner with a narrow therapeutic window. Too little, and you risk a clot. Too much, and you bleed internally. For drugs like this, regulators tighten the range to 90-111%. One small change in absorption can make a life-or-death difference. Bioequivalence testing catches those risks before a drug even hits the shelf.
How Testing Is Done (And Why It’s Not Simple)
Most bioequivalence studies happen in healthy volunteers-not patients. Why? Because you need clean data. If someone has liver disease, kidney issues, or is on other meds, it muddies the results. So researchers recruit people aged 18-65, with normal BMI (18.5-30 kg/m²), no major health conditions, and no recent drug use. They fast overnight, then take a single dose of either the brand or generic drug. Blood is drawn every 15-30 minutes for 24-72 hours. The process is repeated a week later, with the other version.This crossover design controls for individual differences. If your body absorbs drug A faster than drug B, and the results still fall within 80-125%, you’ve got bioequivalence. But it’s not just about the numbers. The lab must use validated methods-like LC-MS/MS-to detect tiny amounts of the drug in blood. If the test can’t measure low concentrations accurately, the whole study is invalid.
And it’s expensive. A single study costs $1-2 million and takes 12-18 months. That’s why only serious companies invest in it. The cost isn’t just for the science-it’s for compliance. Every step must follow FDA, EMA, or ICH guidelines. Deviate, and the drug gets rejected.
When the Rules Get Tricky: Highly Variable and Complex Drugs
Not all drugs play nice. Some, like certain antibiotics or epilepsy meds, vary wildly from person to person. One person’s Cmax might be 150 ng/mL; another’s might be 400 ng/mL-even with the same dose. That’s called high within-subject variability. The old 80-125% rule would fail these drugs, even if they’re perfectly safe.That’s why regulators created scaled average bioequivalence (SABE). For these drugs, the acceptable range widens to 75-133%, but only if the drug’s own variability is high enough (over 30%). And there’s a catch: the geometric mean ratio (GMR) can’t stray too far from 100%. This prevents a drug that’s consistently 130% stronger from slipping through.
Then there are complex products: inhalers, topical creams, eye drops. You can’t just measure blood levels. For a steroid cream, you need to know how much gets into the skin. For an inhaler, how much reaches the lungs? These require special tests-sometimes in-vitro (lab-based), sometimes in-vivo (in patients). The EMA’s 2023 update on topical products added new standards for how these are tested. The FDA’s 2022 initiative on complex generics is doing the same. It’s not easy. Dr. Lawrence Yu of the FDA called topical dermatologicals “one of the most difficult challenges in generic development.”

Biosimilars vs. Generics: A Common Confusion
People often think all generics are the same. But there’s a big difference between small-molecule generics and biosimilars. Generics are chemically identical copies of simple drugs like metformin or lisinopril. Their bioequivalence is proven through blood tests.Biosimilars? They’re copies of complex biologic drugs-like Humira or Enbrel. Made from living cells, not chemicals. They’re not identical. Even tiny changes in manufacturing can alter how they behave. So regulators don’t rely on bioequivalence alone. They use a “totality of evidence” approach: structural analysis, animal studies, immune response tests, and clinical trials. It’s far more complex than testing a pill.
That’s why biosimilars cost more and take longer to approve. But they’re still cheaper than the original biologics. And yes-they’re safe, when tested properly.
Does It Actually Work? Real-World Evidence
You might have heard stories: “I switched to generic sertraline and felt awful.” Or “My thyroid med didn’t work after the switch.” These anecdotes are real to the people who experience them. But they’re not proof of failure.The FDA tracks adverse events through FAERS. From 2020-2023, only 0.07% of all reports involved bioequivalent generics. Brand-name drugs? 2.3%. That’s a 30-fold difference. If generics were unsafe, we’d see a spike. We don’t.
A 2022 survey by the National Community Pharmacists Association found 87% of U.S. patients said generics worked just as well as brand names. On Drugs.com, generic levothyroxine has a 6.5/10 rating. Yes, some people complain-but 58% say it works the same. The rest often blame the switch itself, not the drug. Placebo effect? No. But psychological bias? Absolutely. When patients are told, “This is generic,” they sometimes expect it to be worse. That can change how they feel.
And here’s the kicker: if a generic drug were truly unsafe, the FDA would pull it. They’ve done it before. In 2012, they tightened standards for levothyroxine after reports of inconsistent absorption. The new bioequivalence rules fixed it. Since then, adverse events dropped. That’s the system working.
Why This Matters for Patient Safety
Generic drugs make up 90% of prescriptions in the U.S. but only 23% of drug spending. In 2020 alone, they saved the system $313 billion. That’s not just a number. It’s people who can afford their insulin. Their blood pressure meds. Their antidepressants.Without bioequivalence testing, we’d have no way to guarantee that these cheap drugs are safe. We’d be flying blind. Imagine a world where you couldn’t trust that your generic aspirin had the same dose as the brand. Or your generic metformin didn’t control your blood sugar. That’s not hypothetical. It happened before regulations were strong.
Bioequivalence isn’t about cutting corners. It’s about setting a high bar-and holding every generic manufacturer to it. Whether it’s a simple tablet or a complex inhaler, the goal is the same: same effect, same safety, same outcome. And for millions of patients, that’s not just science-it’s survival.
What’s Next for Bioequivalence?
The field is evolving. The FDA now accepts 17 submissions using PBPK modeling (physiologically-based pharmacokinetics) to predict how a drug will behave-without running full human trials. That’s a big deal. It could cut costs and speed up access.AI is also being explored. Can we predict bioequivalence from dissolution profiles? Early results look promising. But regulators are cautious. Human data still matters most.
And globally, the trend is clear. In 2015, 89 countries had bioequivalence requirements. By 2023, that number jumped to 134. The WHO, EU, U.S., Australia, Canada, Japan-all agree. This isn’t optional. It’s essential.
As complex drugs become more common, the science will keep adapting. But the mission won’t change: protect patients. Ensure safety. Make medicine affordable. Bioequivalence testing is how we do all three.
Is a generic drug always as safe as the brand-name version?
Yes-if it passes bioequivalence testing. The FDA and EMA require that generics meet strict standards for how much drug enters the bloodstream and how fast. If the drug is bioequivalent, it’s considered therapeutically equivalent. Adverse event data from the FDA shows generic drugs with proven bioequivalence have far fewer safety issues than brand-name drugs, suggesting the system works.
Why do some people say generic drugs don’t work for them?
Anecdotal reports are common, especially with drugs like antidepressants or thyroid meds. But these cases rarely reflect true bioequivalence failure. Psychological factors, changes in filler ingredients, or even switching between different generic manufacturers can cause perceived differences. The FDA tracks these reports closely and would recall a product if a pattern of harm emerged. Real failures are extremely rare.
Are all generic drugs tested the same way?
No. Simple pills are tested with blood samples in healthy volunteers. But for complex products like inhalers, creams, or eye drops, different methods are needed. Some require in-vitro testing or patient studies. For highly variable drugs, regulators use adjusted standards. The method depends on the drug’s properties, not just its form.
What’s the difference between a generic and a biosimilar?
Generics are exact chemical copies of small-molecule drugs like aspirin or metformin. They’re proven bioequivalent through blood tests. Biosimilars are copies of complex biologic drugs like Humira, made from living cells. They’re not identical, so they require more testing-structural analysis, immune response studies, and clinical trials. Bioequivalence alone isn’t enough for biosimilars.
Can switching between generic brands cause problems?
In rare cases, switching between different generic versions of the same drug can cause issues, especially with narrow therapeutic index drugs like warfarin or levothyroxine. That’s why pharmacists and doctors sometimes recommend sticking to one generic brand. But this isn’t because the generics are unsafe-it’s because each manufacturer’s formulation may have slight differences in fillers or release profiles. Bioequivalence ensures each version is safe on its own, but switching between them isn’t always predictable for sensitive patients.


steve rumsford
Generic drugs saved my ass when I lost my insurance. I was on brand-name antidepressants that cost $400 a month. Switched to generic, paid $12, felt the same. No drama. No side effects. Just science working the way it should.
People who say it doesn’t work? Probably just stressed about the change, not the pill.