When a patient walks in with a prescription for a brand-name drug, and their insurance pushes for a generic, what do you say? Many doctors still hesitate-even though 90% of prescriptions filled in the U.S. are for generics. The problem isn’t science. It’s misinformation. Patients worry generics aren’t as strong. Some doctors secretly believe it too. That’s why prescriber education resources aren’t optional-they’re essential.
Why Doctors Still Doubt Generics
It’s not that doctors don’t trust science. It’s that they’re bombarded with conflicting messages. A 2023 survey found 68% of physicians found FDA generic guides useful-but too technical to use during a 10-minute visit. One doctor in Nebraska told me she used to prescribe brand-name statins to elderly patients who’d say, ‘My cousin took the generic and felt awful.’ She didn’t know how to respond. Then she saw the FDA’s infographic showing how both brand and generic versions are made in the same FDA-inspected facilities, with the same active ingredients, same dosage, same release profile. Her prescribing rate jumped from 62% to 89% in 18 months. The real barrier isn’t clinical knowledge. It’s time. A 2022 study in Annals of Internal Medicine found 73% of physicians said they simply didn’t have time to dig through PDFs during a busy clinic day. And most EHR systems don’t integrate these resources. You’re expected to remember bioequivalence ranges (80-125%) while juggling three other patients, a refill request, and a confused spouse asking why the pill looks different.What the FDA Actually Says About Generics
The FDA doesn’t just approve generics-they test them. Every single one. To get approval, a generic must prove it delivers the same amount of active ingredient into the bloodstream at the same rate as the brand. That’s not theory. It’s measured in clinical studies with 24-36 healthy volunteers. The 80-125% range isn’t a loophole-it’s a statistical confidence interval that ensures therapeutic equivalence. A 2022 analysis of 12,467 adverse event reports for generics showed no higher risk than brand-name drugs. The FDA’s 2022 Prescriber Flyer (Version 2) breaks this down in plain language. It’s a single page. Fits in a waiting room rack. Includes a QR code linking to Spanish-language resources because 42% of Hispanic patients express more concern about generic quality than non-Hispanic white patients. And it’s written at a 6th-8th grade reading level. No jargon. No Latin terms. Just facts.The Cost Difference Isn’t Small-It’s Life-Changing
Dr. Aaron Kesselheim from Harvard put it simply: ‘For a $300/month brand-name medication, switching to generic saves the patient $262.50 monthly.’ That’s not a discount. That’s a lifeline. CMS data from 2020 shows patients earning under $25,000 a year are 3.7 times more likely to stop taking essential meds because they can’t afford them. A study from the Institute for Clinical and Economic Review found that brand-name overuse due to prescriber misconceptions costs the U.S. system $1.3 billion annually. That’s not just waste. That’s preventable hospitalizations, ER visits, and complications. The American College of Physicians has been clear since 2015: ‘All clinicians should prescribe generic medications whenever possible as a way to improve adherence to therapy.’ And they’re right. When patients can afford their meds, they take them. When they take them, outcomes improve. It’s that simple.
What’s Missing from Most Education Materials
The FDA’s toolkit has 12 social media templates, 5 customizable info cards, and 3 infographics. Great. But if you’re in a clinic with no internet, no printer, and 12 patients back-to-back, none of that helps. The biggest gap? Integration. Only 37% of major EHR systems like Epic or Cerner have pop-ups or alerts that push generic education content directly into the workflow. One doctor on Reddit said it best: ‘I need this info in my Epic alert box, not as a PDF I have to hunt for.’ Kaiser Permanente fixed this. In 2021, they embedded FDA generic facts into their Epic system. Within six months, brand-name prescribing dropped by 18.7%. That’s not magic. That’s smart design. When the right info shows up at the right time, behavior changes.Complex Generics Are the New Frontier
It’s easy to explain a generic pill. It’s harder to explain a generic inhaler, topical cream, or injectable. These are called ‘complex generics’-and they make up 22% of prescriptions. Bioequivalence is trickier here. Dissolution rates, particle size, delivery mechanisms-all matter. The European Medicines Agency (EMA) teaches this differently than the FDA. They focus on comparative dissolution profiles. The U.S. still leans on pharmacokinetic studies. But both agree on one thing: the drugs work the same. The difference is in how they’re taught. And that’s where confusion creeps in. Even worse? Authorized generics. These are brand-name drugs sold under a generic label-same factory, same formula, same packaging, just cheaper. A 2023 University of Arizona study found 61% of physicians didn’t even know they existed. That’s a gap in trust. If a patient gets a pill that looks exactly like the brand, but costs half as much, and the doctor didn’t explain it, they’ll assume it’s inferior.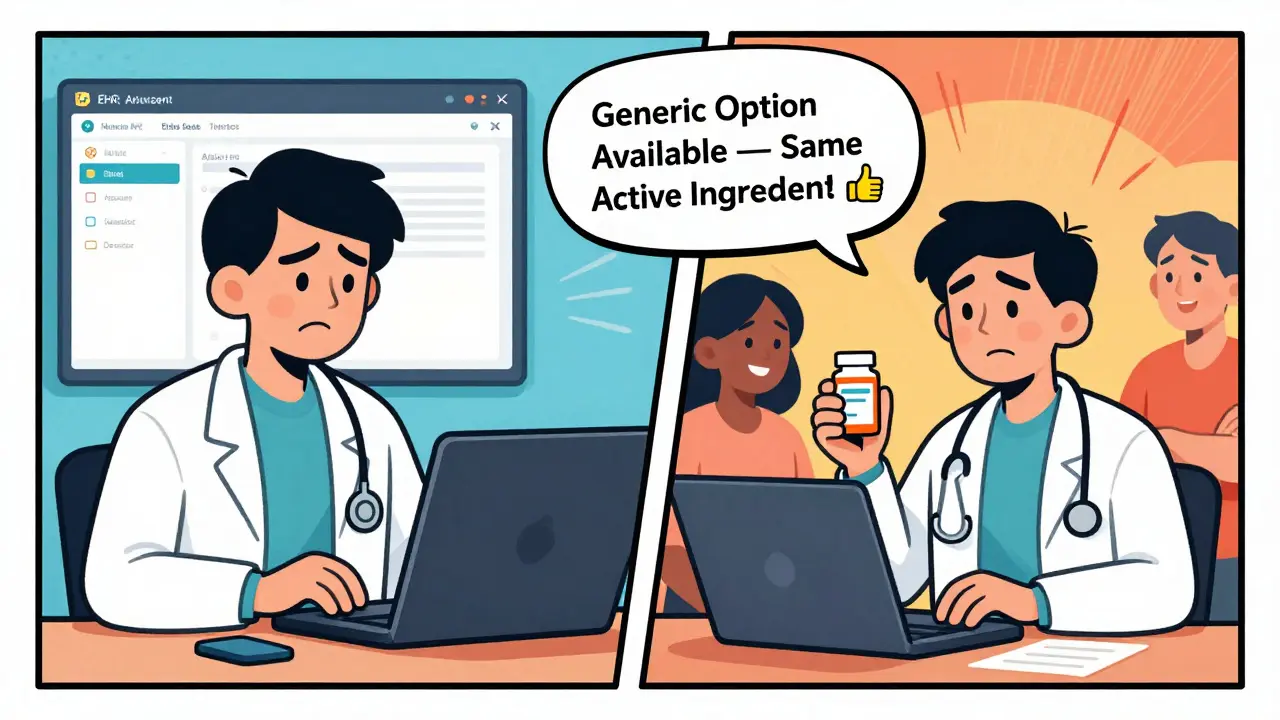
How to Start Using These Resources Today
You don’t need a grant or a hospital IT team. Here’s how to begin:- Download the FDA Prescriber Flyer (Version 2)-it’s 142 KB, free, and printable. Keep one on your desk.
- Use the ‘What Makes a Generic the Same?’ infographic during visits. Show it on your tablet. Point to the manufacturing facility comparison.
- Practice a simple script: ‘This generic has the same active ingredient, same dose, same effect. The only difference is the price. It’s been tested just as strictly.’
- Track your own prescribing rate. If you’re prescribing generics at 70%, aim for 80%. Small shifts add up.
- Ask your EHR vendor if they can integrate FDA generic alerts. If they say no, ask again next quarter.
What Works for Other Doctors
A rural family physician in Nebraska saw her generic prescribing jump from 62% to 89% after using the FDA infographic. She didn’t change her training. She just showed patients the truth. A large health system in Ohio reduced brand-name opioid prescriptions by 22% after integrating CDC’s generic substitution guidance into their pain management protocol. A group of primary care doctors in Texas started a monthly 15-minute ‘Generic Roundtable’-no slides, just questions. ‘What’s the most common concern you hear?’ ‘How do you explain it?’ Within six months, their generic prescribing rate hit 91%. The pattern? It’s not about more education. It’s about better access. Simpler tools. Real conversations.The Future Is Personalized
IBM Watson Health tested an AI tool in 2023 that generated personalized generic substitution messages based on patient history, income, and previous concerns. In a trial with 120 physicians, patient acceptance of generics jumped 29 percentage points. That’s not science fiction. That’s the next step. Medicare’s 2024 proposed rule includes financial incentives for plans that support prescriber education on therapeutic alternatives. That means more funding, more tools, more pressure to act. The data is clear: generics are safe, effective, and life-saving. The only thing holding us back is outdated assumptions and poor integration. You don’t need to be a pharmacologist. You just need to know the facts-and have a way to share them quickly. The tools are there. The science is solid. The patients are waiting.Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also demonstrate bioequivalence-meaning they deliver the same amount of drug into the bloodstream at the same rate. Studies show generic drugs work just as well in real-world use, with no difference in effectiveness or safety.
Why do some patients refuse to take generics?
Many patients believe generics are lower quality because they look different or cost less. Others have heard stories from friends or family about bad experiences. Some assume the brand-name version is ‘stronger.’ These are myths. The FDA’s educational materials use visuals and simple language to explain that manufacturing standards are identical, and the only difference is price and inactive ingredients like color or shape.
Can I trust generics from other countries?
In the U.S., all generics-whether made domestically or imported-must meet FDA standards. The FDA inspects foreign manufacturing sites just like U.S. ones. If a generic is sold legally in the U.S., it’s been reviewed and approved. Be cautious of online pharmacies selling drugs without FDA approval, but FDA-approved generics, regardless of origin, are safe.
Do generics have the same side effects as brand-name drugs?
Yes. Since generics contain the same active ingredient and are absorbed the same way, their side effect profile is identical. The FDA reviews adverse event reports for both brand and generic versions. In 2022, there were 12,467 reports for generics and 11,832 for brand-name drugs-no significant difference in safety.
Why don’t EHR systems show generic education tools automatically?
Most EHR systems were built before generic education became a priority. Integration requires technical work and vendor cooperation. Only 37% of major systems currently include FDA generic prompts. But some health systems like Kaiser Permanente have successfully added them-and seen prescribing rates rise. Doctors can push their EHR vendors to include these tools as a standard feature.
What’s the difference between a generic and an authorized generic?
An authorized generic is made by the original brand-name manufacturer and sold under a generic label. It’s identical to the brand-same factory, same formula, same packaging. The only difference is the price. Many doctors don’t know these exist, and patients often don’t realize they’re getting the exact same drug. Explaining this can ease concerns and improve trust.
Are there any drugs where generics aren’t recommended?
For most drugs, generics are equally effective. But for a small number of complex medications-like certain inhalers, topical creams, or injectables-small differences in delivery can matter. Even then, FDA-approved generics are still safe and effective. The key is not avoiding generics, but understanding the specific drug class. Resources like the FDA’s Generic Drugs Stakeholder Toolkit include guidance for these cases.
How long does it take to get comfortable prescribing generics?
A 2022 clinical trial showed physicians need about 22 minutes of focused education to overcome initial skepticism. That’s less than two patient visits. The key is not memorizing data-it’s learning how to explain it simply. Once you’ve used the FDA’s scripts and visuals a few times, it becomes second nature.
Do insurance companies force doctors to prescribe generics?
Insurance plans often require patients to try generics first, but doctors still have final prescribing authority. You can override a prior authorization if you believe the brand is medically necessary. But if the generic is appropriate, prescribing it saves the patient money and improves adherence. Most patients appreciate the cost savings when they understand it’s the same medication.
Where can I find the most reliable generic drug resources?
The FDA’s Generic Drugs Education Program offers the most authoritative, up-to-date materials, including the Prescriber Flyer, Stakeholder Toolkit, and infographics-all free and downloadable at fda.gov/generics. Other trusted sources include the American College of Physicians and the CDC’s prescribing guidelines. Avoid commercial websites or pharmaceutical marketing materials-they’re not designed to educate objectively.



Haley Graves
The FDA flyer is a game-changer. I keep a printed copy on my desk and pull it out when patients worry about the color or shape of the pill. One elderly woman cried when she realized her cousin’s bad experience wasn’t because the generic was weaker-it was because she took it with grapefruit juice. Simple visuals, real talk. That’s all it takes.