Black Box Risk Assessment Tool
Personal Risk Assessment
Answer these questions to understand potential risk factors related to medications with black box warnings. This tool does not diagnose or replace professional medical advice.
Risk Assessment Results
Key Risk Factors Identified:
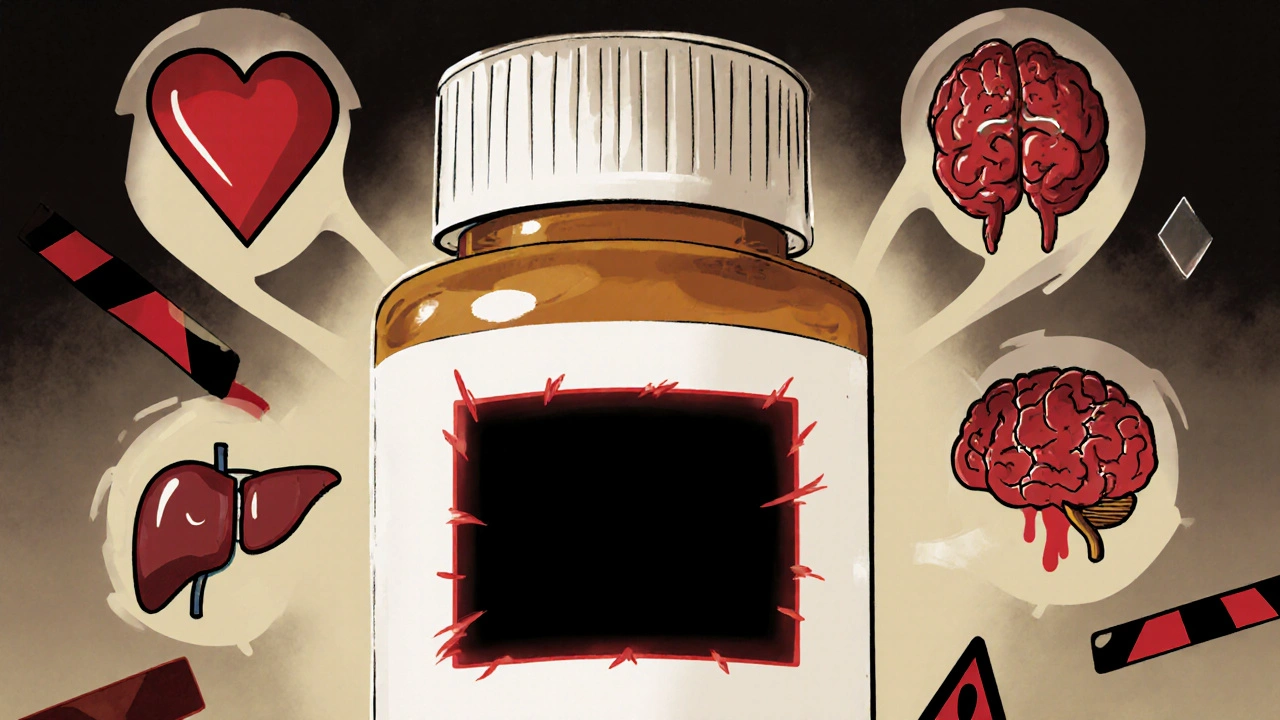
When you pick up a prescription, you probably don’t expect to see a warning that could save your life-or warn you away from taking it altogether. But for more than 400 medications on the market, that’s exactly what’s printed in bold black borders at the very start of the drug’s label. These are black box warnings, the FDA’s most serious safety alert. They don’t just say "use with caution." They say: "This drug can kill you if used wrong."
What Exactly Is a Black Box Warning?
A black box warning is a mandatory label the U.S. Food and Drug Administration requires on certain prescription drugs. It’s not a footnote. It’s not a small print notice tucked at the bottom of a pamphlet. It’s a thick black rectangle-like a border around a grim photograph-placed right after the drug’s name and before any other information in the prescribing guide. Inside that box, you’ll find a blunt, no-nonsense summary of the most dangerous risks linked to the drug: things like sudden heart failure, severe liver damage, suicidal thoughts, or death. These warnings aren’t added lightly. The FDA only puts them on drugs when multiple studies show a clear, serious, and sometimes preventable risk. The system started in the 1960s after the thalidomide tragedy, but the black box format as we know it today became standard in the 1980s. Today, it’s the highest level of warning the FDA has. Nothing else on a drug label carries this weight-not even the "Warnings and Precautions" section that follows it.Why Do These Warnings Exist?
The goal isn’t to scare people off medicine. It’s to make sure no one takes a high-risk drug without fully understanding the stakes. Some drugs are essential for treating life-threatening conditions-like cancer, severe depression, or autoimmune diseases-but they come with brutal side effects. A black box warning forces doctors and patients to pause, ask hard questions, and weigh the risks against the benefits. For example, antidepressants like fluoxetine and sertraline carry black box warnings about increased suicidal thoughts in young adults under 25. That doesn’t mean you shouldn’t take them. It means if you’re 19 and starting treatment, your doctor needs to monitor you closely in the first few months. Or take the diabetes drug rosiglitazone, which got a black box warning for heart attack risk. After the warning, prescriptions dropped by 70%. But here’s the catch: another similar drug, pioglitazone, had a similar warning but didn’t see the same drop-because it didn’t get the same media attention. The warning alone isn’t enough. Awareness matters.When Does the FDA Decide to Add a Black Box Warning?
The FDA doesn’t slap these on during drug approval. Most black box warnings come after a drug is already on the market. That’s because some risks only show up when thousands or millions of people use the drug over years. Post-market surveillance catches what clinical trials miss. The FDA looks at three main triggers before adding a black box warning:- The risk is so severe that it could outweigh the drug’s benefits for some patients.
- The side effect can be reduced-if the patient is monitored, avoids certain other drugs, or follows strict dosing rules.
- There’s a specific group of people who should never take the drug-like pregnant women, people with liver disease, or those with a history of certain heart conditions.
What Do These Warnings Actually Say?
Each black box warning is written in plain language-but it’s dense. Here’s what you’ll typically find inside:- Specific danger: "Risk of severe liver injury, including fatal hepatitis."
- Who’s at risk: "Patients with pre-existing liver disease."
- What to avoid: "Do not use with alcohol or other hepatotoxic drugs."
- Monitoring needed: "Check liver enzymes every 2 weeks for the first 3 months."
- Contraindications: "Not recommended for patients with a history of pancreatitis."
How Do Doctors Use These Warnings?
Doctors don’t just glance at the box and move on. Experts recommend using a framework called STEPS: Safety, Tolerability, Effectiveness, Price, Simplicity. When a drug has a black box warning, "Safety" becomes the top priority. A good doctor will:- Check your medical history for red flags (like kidney disease, heart problems, or past reactions to similar drugs).
- Review all your other medications to avoid dangerous interactions.
- Discuss alternatives-maybe there’s a safer drug that works just as well.
- Set up follow-up tests or check-ins to catch early signs of trouble.
What Should You Do If Your Drug Has a Black Box Warning?
Don’t panic. Don’t stop taking it without talking to your doctor. But do this:- Ask for the full warning text. Don’t rely on your memory or a nurse’s summary. Get the exact wording from the prescribing guide.
- Know your risk factors. Are you in the group the warning warns about? If so, what’s the plan to manage it?
- Ask about alternatives. Is there another drug without the same risk? Is there a non-drug option?
- Track symptoms. If the warning mentions dizziness, fatigue, or jaundice, write down when they happen and tell your doctor.
- Report side effects. Use the FDA’s MedWatch portal to report anything unusual-even if you’re not sure it’s related. Your report could help protect someone else.
Are Black Box Warnings Effective?
Sometimes. Sometimes not. The rosiglitazone example shows that warnings work best when they’re backed by media coverage, doctor education, and patient awareness. But many patients never even see the warning. The label is printed in tiny font inside the pill bottle. Most people don’t read it. That’s why the FDA is exploring better formats-like clearer language, visual icons, or even digital alerts when a prescription is filled. Studies show that black box warnings reduce prescribing for the warned-about drug-but not always for the right reasons. Sometimes doctors avoid the drug because they’re scared, not because they’ve done a real risk-benefit analysis. Other times, they prescribe it anyway because the patient has no other options. The bottom line: the warning is a tool. It’s only as good as the conversation around it.What’s Next for Black Box Warnings?
The FDA is working on making these warnings more useful. In 2011, they updated their guidance to require clearer language and better organization. Now, they’re pushing for more patient-centered design. Instead of saying "risk of death," they might say "1 in 500 patients may die from this side effect." Numbers stick better than vague terms. There’s also growing pressure to make warnings public faster. Right now, the FDA often waits months or years to update a warning after new data comes in. Advocacy groups are pushing for real-time updates tied to the FDA’s adverse event database, FAERS. But the core idea remains unchanged: some drugs are powerful enough to heal-and to harm. The black box is the FDA’s way of saying: "This isn’t ordinary medicine. Treat it like a scalpel, not a candy."Do all prescription drugs have black box warnings?
No. Only about 400 out of thousands of prescription drugs carry black box warnings. These are reserved for medications with serious, potentially life-threatening risks that require special caution. Most common drugs-like antibiotics, blood pressure pills, or allergy meds-don’t need them.
Can I still take a drug with a black box warning?
Yes, if your doctor believes the benefits outweigh the risks. Many people take drugs with black box warnings safely-for example, chemotherapy agents, antipsychotics, or immunosuppressants after organ transplants. The warning doesn’t mean the drug is banned or useless. It means you and your doctor need to be extra careful.
How do I find out if my medication has a black box warning?
Check the drug’s prescribing information, usually available online from the manufacturer or through the FDA’s website. Your pharmacist can also show you the full label. Look for a thick black border at the beginning of the document. If you’re unsure, ask your doctor or pharmacist to point it out.
Can a black box warning be removed?
Yes. If new data shows the risk is lower than originally thought-or if safer use practices have reduced harm-the FDA can remove or modify the warning. For example, some older warnings about birth control pills were updated or removed as research improved our understanding of risk factors.
Do over-the-counter drugs have black box warnings?
No. Black box warnings only apply to prescription drugs. Over-the-counter medications have different labeling rules and may carry "Warnings" or "Precautions," but never the FDA’s black box format.


Erin Nemo
Just took my first black box drug last month-sertraline. Scared the crap outta me at first, but my doc sat down and walked me through it. Turns out, the warning’s there so I don’t ignore the red flags. I check in every two weeks now. Feels weird, but kinda empowering.