For decades, women have been told: antibiotics can make your birth control pills useless. If you’ve ever been handed a warning slip at the pharmacy or seen a red flag pop up on a drug interaction checker, you’re not alone. But here’s the truth: most antibiotics don’t touch your birth control. The fear isn’t just outdated-it’s mostly wrong. And yet, it still sticks. Why? Because one antibiotic does, and the confusion has spread like wildfire.
Only One Class of Antibiotics Actually Breaks Birth Control
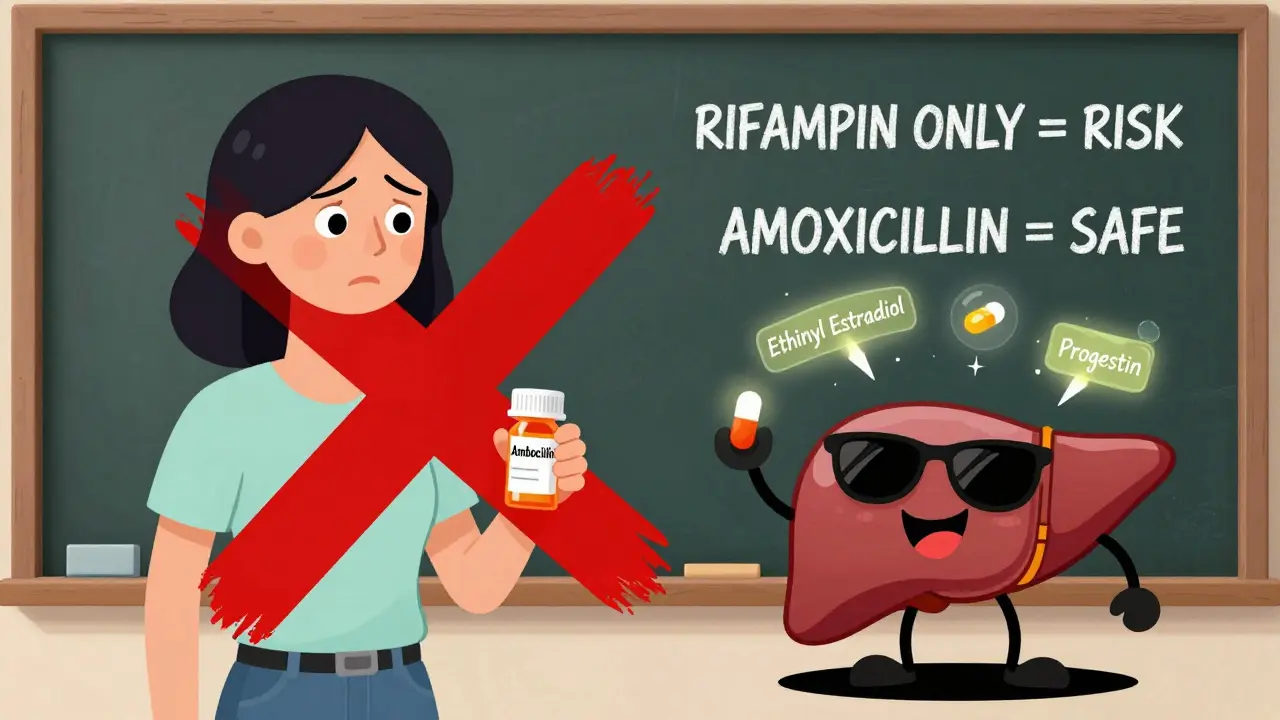
Let’s cut through the noise. There are thousands of antibiotics out there. Amoxicillin? Azithromycin? Doxycycline? Metronidazole? None of them interfere with hormonal birth control. Not in any meaningful, measurable way. The only antibiotics proven to reduce the effectiveness of birth control pills are rifampin (also called rifampicin) and rifabutin. Both are used to treat tuberculosis and some serious bacterial infections. They’re not common. You won’t get them for a sinus infection or a UTI.
Here’s how they work: rifampin and rifabutin are enzyme inducers. That means they crank up your liver’s ability to break down hormones. Specifically, they speed up the metabolism of ethinyl estradiol and progestin-the two key hormones in most birth control pills. Studies show rifampin can slash estrogen levels by 25-50% and progestin by 14-37%. That’s enough to drop hormone concentrations below the threshold needed to prevent ovulation. The CDC classifies this as a category 3 interaction: risks outweigh benefits. That’s why they recommend using a backup method like condoms for 28 days after finishing rifampin.
What About All the Other Antibiotics?
Think about the antibiotics you’ve actually been prescribed. Amoxicillin for strep throat? Azithromycin for a chest infection? Cipro for a UTI? Doxycycline for acne? None of these touch your birth control. A 2011 systematic review in Contraception analyzed 14 studies and found no drop in hormone levels with penicillin-type antibiotics. A 2020 CDC analysis of 35 clinical trials confirmed the same: non-rifamycin antibiotics don’t bring hormone levels below 50 pg/mL-the level at which birth control starts to fail.
Even broad-spectrum antibiotics like ciprofloxacin, clarithromycin, and metronidazole? Zero effect. A 2018 study in Pharmacotherapy tracked women taking amoxicillin while on birth control. Their hormone levels stayed solid. No spikes, no drops. The myth that antibiotics kill gut bacteria and stop estrogen absorption? That theory was debunked years ago. Your body absorbs estrogen through the intestines, but not in a way that’s disrupted by normal antibiotic use. The gut flora changes during antibiotic treatment, but not enough to matter.
Griseofulvin Is the Odd One Out
Griseofulvin isn’t an antibiotic-it’s an antifungal. But it’s often lumped in with antibiotics because it’s used to treat fungal infections like ringworm or athlete’s foot. And yes, it also induces liver enzymes. So if you’re taking griseofulvin for a stubborn fungal infection, you need backup contraception for a full month after finishing it. This is rarely discussed, but it’s real. WebMD and the CDC both list it as a confirmed interaction. If you’re on this drug, don’t assume your birth control is still working.
Other Drugs That Actually Do Interfere
While antibiotics rarely cause problems, other common medications do. If you’re on any of these, your birth control might not be enough:
- Lamotrigine (for epilepsy or bipolar disorder) at doses over 300 mg/day
- Topiramate (for seizures or migraines) at doses over 200 mg/day
- Efavirenz and nevirapine (for HIV treatment)
- St. John’s wort (the herbal supplement for depression)
St. John’s wort is especially sneaky. A 2017 study in Clinical Pharmacology & Therapeutics found it can drop estrogen levels by up to 57%. That’s worse than rifampin. If you’re taking this supplement, your birth control is at risk-even if you’re not on any antibiotics.
Why Does the Myth Still Exist?
It started with case reports in the 1970s. A few women got pregnant while on antibiotics and birth control. Back then, birth control pills had much higher hormone doses. But the real culprit? Missed pills, vomiting, diarrhea, or using rifampin without knowing. The media ran with the story. Pharmacists kept warning patients. And now, decades later, it’s still going.
A 2022 Planned Parenthood survey of 1,500 women found 62% believed antibiotics reduced birth control effectiveness. Even more alarming: 43% had used backup contraception during antibiotic treatment-despite no medical need. Meanwhile, a 2022 study in the Journal of the American Pharmacists Association found 35% of pharmacists still advise backup contraception for all antibiotics. That’s not just outdated-it’s misleading.
Dr. Jen Gunter, an OB/GYN and author of The Menopause Manifesto, puts it bluntly: “There’s zero evidence that common antibiotics like amoxicillin affect birth control.” Dr. Eve Espey, former chair of ACOG’s Committee on Gynecologic Practice, says the myth persists because early case reports weren’t scientifically rigorous. But the science now is crystal clear.
What Should You Do?
Here’s your simple guide:
- If you’re prescribed rifampin or rifabutin: Use condoms or another barrier method for 28 days after your last dose.
- If you’re prescribed griseofulvin: Use backup contraception for 30 days after finishing.
- If you’re prescribed any other antibiotic-amoxicillin, azithromycin, doxycycline, cipro, metronidazole, etc.-your birth control is still working. No backup needed.
- If you’re on lamotrigine, topiramate, efavirenz, nevirapine, or St. John’s wort: Talk to your doctor about switching or adding backup contraception.
And if your pharmacist tells you to use condoms with amoxicillin? You’re not wrong to ask for proof. Ask them to check the CDC’s 2021 US Medical Eligibility Criteria. Or pull up ACOG’s 2022 Practice Bulletin. Both say the same thing: no backup needed for non-rifamycin antibiotics.

What About the Patch or Ring?
Same rules apply. Whether you’re on the pill, the patch (Xulane), or the vaginal ring (NuvaRing), only rifampin, rifabutin, and griseofulvin affect them. The CDC’s guidelines apply to all combined hormonal contraceptives. So if you’re on the patch and get prescribed rifampin? Use condoms for 28 days. If you’re on the ring and get amoxicillin? No change needed.
What If You’re on Birth Control and Get Sick?
Diarrhea or vomiting for more than 48 hours? That’s a different issue. If you throw up within two hours of taking your pill, treat it like a missed dose. Same if you have severe diarrhea-it can reduce absorption. In those cases, use backup contraception for the next seven days. But that’s not because of the antibiotic. That’s because your body didn’t absorb the hormone.
What’s Changing in 2026?
The FDA updated labeling for all hormonal contraceptives in January 2023 to clearly state: “Rifampin, rifabutin, and griseofulvin may reduce effectiveness. Other antibiotics do not affect effectiveness.” This is huge. It’s now official. Drug manufacturers have to say it plainly on packaging.
Research is shifting too. The National Institutes of Health now prioritize studying whether obesity affects how rifampin interacts with birth control. Women with a BMI over 30 already have a 2.5 times higher risk of contraceptive failure-even without antibiotics. That’s the real frontier now: personalizing contraception for body composition, not just drug labels.
For now, the message is simple: Don’t panic when you get an antibiotic prescription. Only three drugs out of hundreds actually matter. And if you’re ever unsure, ask your doctor: “Is this one of the ones that affects birth control?” If they hesitate, they might be stuck in the old myth. You now have the facts.
Do all antibiotics make birth control pills less effective?
No. Only rifampin, rifabutin, and griseofulvin have been proven to reduce the effectiveness of hormonal birth control. Common antibiotics like amoxicillin, azithromycin, doxycycline, and metronidazole do not interfere with birth control pills, patches, or rings.
What should I do if I’m prescribed rifampin while on birth control?
Use a backup method like condoms or a diaphragm for 28 days after your last dose of rifampin. This applies to all combined hormonal contraceptives, including pills, patches, and vaginal rings. The CDC and ACOG both recommend this to prevent unintended pregnancy.
Can I trust my pharmacist if they say I need backup contraception with amoxicillin?
You can ask them to check the CDC’s 2021 US Medical Eligibility Criteria or ACOG’s 2022 guidelines. Both state that non-rifamycin antibiotics like amoxicillin do not reduce birth control effectiveness. Many pharmacists still give outdated advice due to lingering myths, but the science is clear: no backup is needed.
Does diarrhea or vomiting affect birth control when I’m on antibiotics?
Yes-but not because of the antibiotic. If you vomit within two hours of taking your pill or have severe diarrhea for more than 48 hours, your body may not absorb the hormones properly. In those cases, use backup contraception for the next seven days. This is a separate issue from drug interactions.
Are there other medications besides antibiotics that can make birth control less effective?
Yes. Lamotrigine (at doses over 300 mg/day), topiramate (over 200 mg/day), efavirenz, nevirapine, and St. John’s wort can all reduce hormone levels. If you’re taking any of these, talk to your doctor about whether you need a different contraceptive method or backup protection.
If you’re on birth control and need antibiotics, the bottom line is this: most of the time, you’re fine. Only a handful of drugs are the real problem. Stop worrying about amoxicillin. Start paying attention to the ones that actually matter.