Vaginal Surgery Procedure Selector
Select a procedure to see detailed information.
Select a procedure to view recovery timeline.
Select a procedure to see key considerations.
When it comes to vaginal surgery, the amount of information online can feel overwhelming. You might be wondering what the procedures actually involve, how long it takes to heal, or whether any risks are worth the benefits. This FAQ‑style guide breaks down the most common questions in plain language, so you can make an informed decision without getting lost in medical jargon.
Vaginal surgery is a group of surgical procedures that modify or repair the vagina and surrounding tissues. These operations address functional issues such as pelvic organ prolapse, incontinence, or discomfort, as well as aesthetic concerns like labial size. The goal is to improve quality of life, restore normal function, and, for many patients, boost confidence.
What types of vaginal surgery are most common?
There are several distinct procedures, each targeting a specific problem. Below is a quick snapshot of the three most frequently performed surgeries.
| Procedure | Primary Goal | Typical Recovery | Key Risks |
|---|---|---|---|
| Labiaplasty | Reduce excess labial tissue for comfort or aesthetics | 2-4 weeks | Infection, scarring, altered sensation |
| Vaginoplasty | tighten the vaginal canal, often after childbirth | 4-6 weeks | Pain, urinary issues, scar tissue |
| Pelvic organ prolapse repair | Restore support to bladder, uterus, or rectum | 6-8 weeks | Recurrence, mesh complications (if used) |
Who performs these surgeries?
Gynecologic surgeon is a medical doctor specialized in women’s reproductive health and trained to conduct vaginal procedures. They may be a board‑certified OB‑GYN or a urologist with additional fellowship training. Choosing a surgeon with extensive experience in the specific operation you need can lower complication rates and improve satisfaction.
What kind of anesthesia is used?
Anesthesia can be either general (you’re asleep) or regional, such as a spinal or epidural block that numbs the lower half of your body while you stay awake. The choice depends on the procedure’s length, your medical history, and personal comfort. Your surgeon will discuss the best option during the pre‑operative visit.
How should I prepare for surgery?
- Attend the pre‑operative appointment and share a complete medical history, including any medications, allergies, and previous surgeries.
- Stop smoking at least two weeks before the operation; nicotine slows healing.
- Follow any fasting instructions-usually nothing solid after midnight before a morning surgery.
- Arrange for a friend or family member to drive you home and help for the first 24 hours.
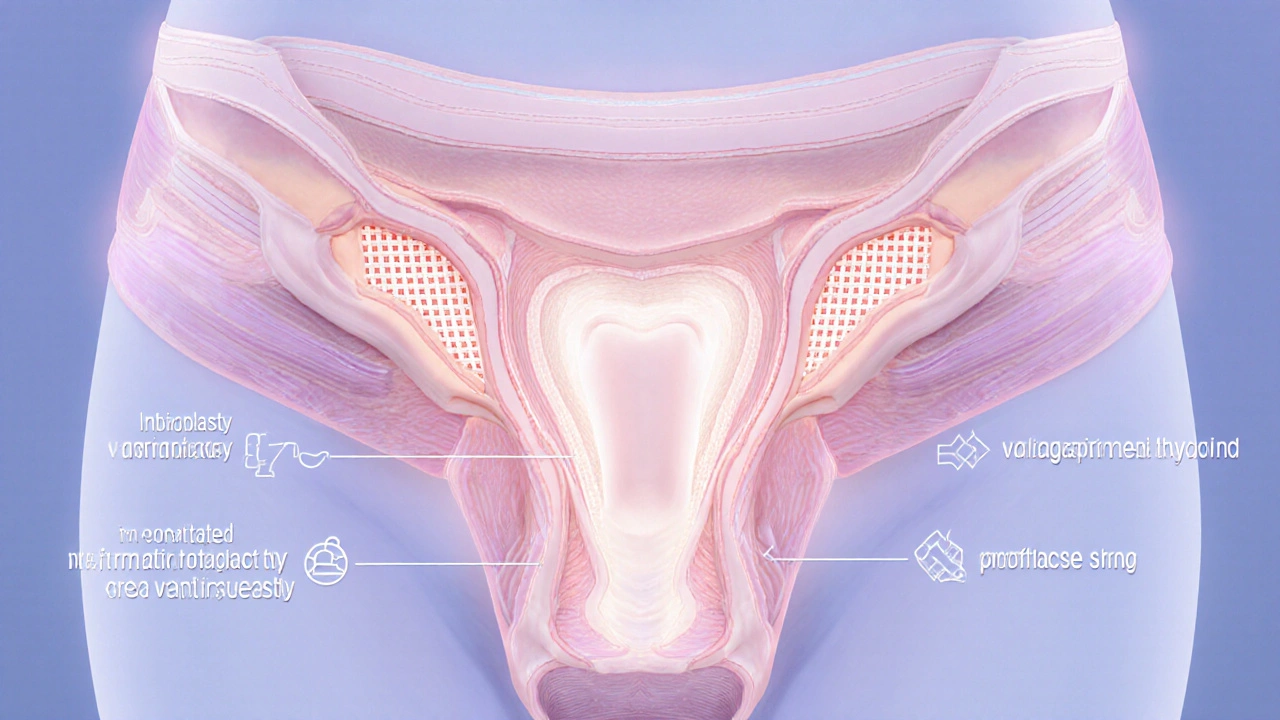
What does the actual surgery involve?
Most vaginal surgeries are performed in an outpatient setting, meaning you can go home the same day. After a brief period of anesthesia, the surgeon makes precise incisions in the vaginal wall or labial tissue, removes or reshapes the targeted area, and then stitches the site with dissolvable sutures. In some prolapse repairs, a supportive mesh may be used, though many surgeons now prefer native‑tissue techniques to avoid mesh‑related complications.
What should I expect during recovery?
Postoperative care focuses on pain control, wound hygiene, and gradual return to normal activities. Most patients experience mild soreness for a few days, which can be managed with prescribed pain relievers or over‑the‑counter ibuprofen. Keeping the area clean-often with a gentle saline rinse-helps prevent infection.
- First 24-48 hours: Rest, keep the perineal area dry, and avoid heavy lifting.
- First week: Light walking is encouraged to improve circulation. Use a peri‑bottle (a small bottle with a nozzle) to rinse after bathroom trips.
- 2-3 weeks: Many people can resume low‑impact exercise. Sexual activity is usually cleared after the surgeon’s follow‑up exam.
- 6-8 weeks: Full activity, including strenuous workouts, is typically safe.
What are the most common complications?
Surgical complications are relatively rare when the procedure is performed by an experienced surgeon. The most frequently reported issues include infection, bleeding, temporary changes in sensation, and scar tissue formation that can cause discomfort. In prolapse repairs that use mesh, there is a small risk of mesh erosion, which may require additional surgery.
How often do results last?
Durability varies by procedure and individual factors such as age, tissue quality, and lifestyle. Labiaplasty and vaginoplasty often provide lasting results for many years, especially when postoperative care recommendations are followed. Pelvic organ prolapse can recur over time; studies show a 10‑15% chance of recurrence within five years, prompting some surgeons to recommend pelvic floor physical therapy as a preventive measure.

Can I combine vaginal surgery with other procedures?
Yes. Some patients opt for a combined approach-such as a labiaplasty together with a hysterectomy-if both are medically indicated. Combining surgeries can reduce overall anesthesia exposure and shorten total recovery time, but it also means a slightly longer operation and more postoperative discomfort. Discuss your goals with the surgeon to weigh the pros and cons.
What should I ask my surgeon during the consultation?
- How many times have you performed this specific procedure?
- What type of anesthesia will be used and why?
- What are the exact risks for someone with my health background?
- How long will I need to stay off work or exercise?
- Will I need any special garments or hygiene products after surgery?
- What follow‑up appointments are required, and what will they involve?
Is vaginal surgery covered by insurance?
Coverage depends on the reason for the surgery. Procedures performed for medical necessity-like prolapse repair or incontinence correction-are usually reimbursed by health plans. Cosmetic‑type surgeries, such as labiaplasty done solely for appearance, are often considered elective and may not be covered. Always verify with your insurer before scheduling.
When should I seek medical attention after surgery?
- Fever over 101°F (38.3°C) that lasts more than 24 hours.
- Increasing pain, swelling, or redness at the incision site.
- Unusual discharge-especially foul‑smelling or bloody beyond the first few days.
- Difficulty urinating or bowel movements that do not improve.
Contact your surgeon’s office promptly if any of these signs appear. Early intervention can prevent more serious problems.
Frequently Asked Questions
How long does a typical vaginal surgery take?
Most outpatient procedures last between 30 minutes and two hours, depending on the complexity. Labiaplasty is usually at the shorter end, while prolapse repair can be longer due to the need for precise tissue reconstruction.
Will I feel pain during the operation?
No. The anesthesia-whether general or regional-ensures you are comfortable throughout the surgery. You may feel pressure or movement, but not pain.
How soon can I return to work?
Most patients resume sedentary or light‑desk work within a week. Jobs that require heavy lifting or prolonged standing may need a two‑to‑four‑week break.
Is sexual activity safe after healing?
Doctors typically clear patients for intercourse after the follow‑up exam, usually around six weeks post‑surgery. Starting gently and using lubrication can help prevent discomfort.
Can vaginal surgery affect future pregnancies?
Procedures that focus on labial or vaginal tightening usually do not interfere with pregnancy or childbirth. However, prolapse repairs that involve deep pelvic tissue may require special counseling if you plan more children. Discuss family‑planning goals with your surgeon beforehand.



Julia Phillips
Reading through this guide felt like stepping into a well‑lit hallway of options. The way you break down each procedure-labia reduction, vaginal tightening, prolapse repair-makes the medical jargon suddenly human. I especially loved the bit about recovery timelines; it takes the fear out of the unknown. For anyone sitting on the fence, this is the map you need.