Azilsartan is an angiotensin II receptor blocker (ARB) used to treat high blood pressure. Unlike some older ARBs, it’s designed to work longer and more consistently throughout the day. But knowing how it works isn’t just about knowing it lowers blood pressure - you need to understand what happens to it inside your body. That’s pharmacokinetics: what your body does to the drug. And for azilsartan, that story matters.
How Azilsartan Gets Into Your Bloodstream
When you swallow an azilsartan tablet, it doesn’t jump straight into your bloodstream. First, it has to survive your stomach acid and get absorbed through the lining of your small intestine. Studies show that azilsartan is absorbed quickly, with peak blood levels reached within 1.5 to 3 hours after taking it. That’s faster than some other ARBs like losartan or valsartan.
Food doesn’t stop azilsartan from working, but it can slow it down a bit. If you take it with a high-fat meal, the time to reach peak levels might stretch to 4 or 5 hours. The total amount absorbed doesn’t drop - you still get the full dose - but the timing changes. For most people, taking it on an empty stomach gives the most predictable results.
One reason azilsartan absorbs well is its chemical structure. It’s more lipophilic than older ARBs, meaning it dissolves better in fats. That helps it slip through the fatty membranes of your gut cells. Once inside, it enters the portal vein and heads straight to the liver.
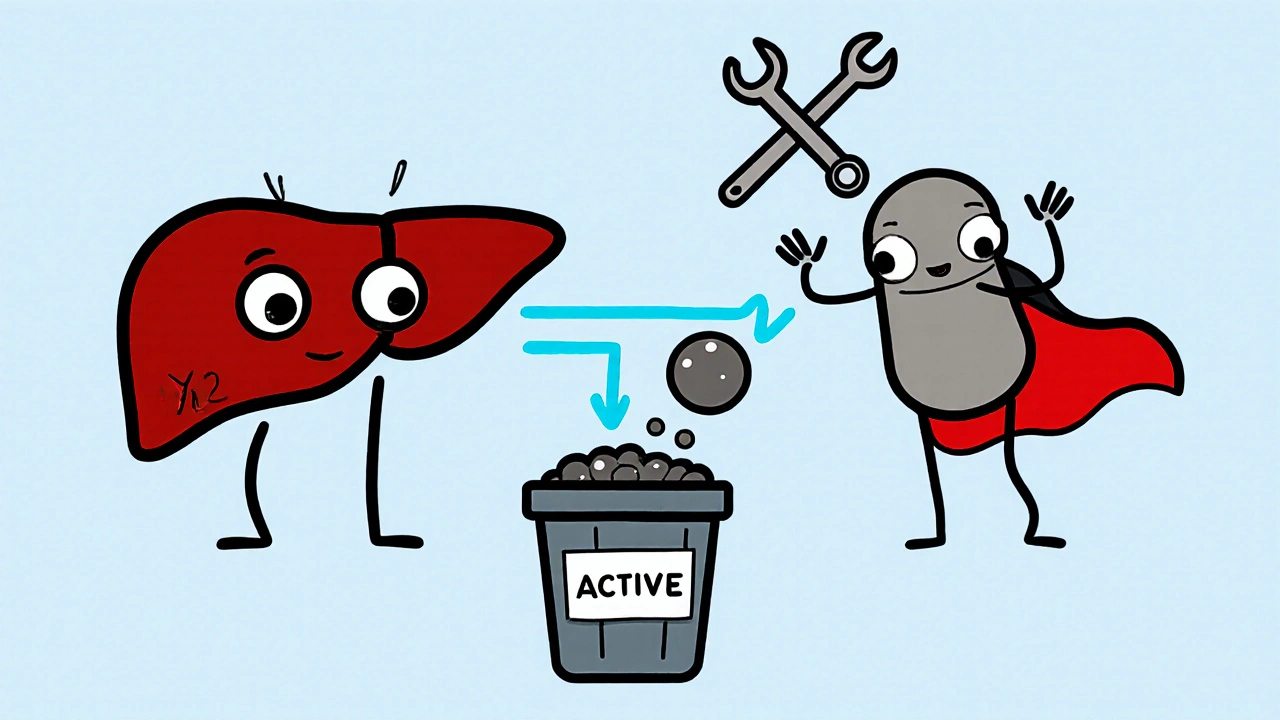
What Happens When Azilsartan Reaches the Liver
The liver is where most drugs get broken down. Azilsartan is no exception, but it doesn’t get destroyed the way some others do. About 60% of the drug passes through the liver unchanged. The rest is metabolized by an enzyme called CYP2C9. This enzyme adds a hydroxyl group to azilsartan, turning it into a minor metabolite called M-II.
Here’s the key point: M-II isn’t active. It doesn’t block angiotensin II receptors. That means almost all the blood pressure-lowering effect comes from the original azilsartan molecule, not its breakdown products. That’s different from drugs like losartan, which turns into an active metabolite. With azilsartan, you’re getting one main player - and it’s the one you took.
Because CYP2C9 is involved, people with genetic variations in this enzyme might process azilsartan a little slower. But studies haven’t shown this leads to major differences in blood pressure control or side effects. So routine genetic testing isn’t needed. If you’re on other drugs that affect CYP2C9 - like fluconazole or amiodarone - your doctor might monitor you more closely, but interactions are rare.
How Long Azilsartan Stays in Your Body
The half-life of azilsartan is about 11 hours. That’s longer than valsartan (6-9 hours) and much longer than losartan (2 hours for the parent drug). But here’s the catch: the half-life doesn’t tell the whole story. Azilsartan’s effect on blood pressure lasts more than 24 hours, even after a single dose.
Why? Because it binds tightly to the angiotensin II receptor. It doesn’t just float in and out - it latches on firmly. This tight binding means even as blood levels drop, the drug is still doing its job. That’s why once-daily dosing works so well. You don’t need two doses to keep your pressure under control.
Some people worry that a long half-life means the drug builds up. But azilsartan doesn’t accumulate in healthy people taking standard doses. After five days of daily use, levels stabilize. If you miss a dose, you won’t suddenly spike your blood pressure. The effect fades slowly.
How Azilsartan Leaves Your Body
Most of azilsartan - about 60% - leaves through your kidneys. The rest goes out in your stool via bile. This dual path is important. If you have kidney disease, your body might clear it a bit slower. But studies show you don’t need to reduce the dose unless your kidney function is severely impaired (eGFR under 30 mL/min).
For people on dialysis, azilsartan can still be used. It’s not removed well by standard hemodialysis, so dosing doesn’t need adjustment. That’s an advantage over some other blood pressure drugs that require dose changes in kidney failure.
There’s no evidence azilsartan builds up in liver disease either. Even in moderate cirrhosis, the drug’s clearance stays mostly unchanged. That’s because most of it is excreted by the kidneys, not the liver.
Why Pharmacokinetics Matter for Real-World Use
Understanding azilsartan’s journey through the body helps explain why it’s prescribed the way it is. The once-daily dose? That’s because of its long receptor binding and 11-hour half-life. The fact that food doesn’t block absorption? That’s why you can take it with or without meals - convenience matters for sticking to treatment.
It also explains why azilsartan works better in some people than other ARBs. In head-to-head trials, it lowered systolic blood pressure by 2-5 mmHg more than valsartan or olmesartan. That small edge comes from better absorption, stronger receptor binding, and no reliance on active metabolites.
For patients with diabetes or chronic kidney disease, azilsartan’s clean pharmacokinetic profile is a plus. No major interactions with common meds like statins, metformin, or diuretics. No need to worry about dose changes in mild to moderate liver or kidney problems. That makes it a practical choice for complex patients.

What You Should Know Before Taking Azilsartan
If you’re prescribed azilsartan, here’s what you need to remember:
- Take it at the same time each day - consistency helps keep blood pressure steady.
- It’s fine to take with food, but if you notice it works slower, try taking it 30 minutes before eating.
- Don’t stop it suddenly. Even though it doesn’t cause rebound spikes like some beta-blockers, stopping abruptly can let your blood pressure rise again.
- Watch for signs of low blood pressure - dizziness, especially when standing up. This is more common if you’re also on diuretics or have low salt intake.
- Let your doctor know if you start or stop any other medications. While interactions are rare, NSAIDs (like ibuprofen) can reduce its effectiveness.
Side effects are generally mild - headache, dizziness, fatigue. Serious reactions like angioedema or kidney injury are rare but possible. If you develop swelling in your face, lips, or throat, seek help immediately.
How Azilsartan Compares to Other ARBs
Here’s how azilsartan stacks up against other common angiotensin II blockers:
| Property | Azilsartan | Valsartan | Olmesartan | Losartan |
|---|---|---|---|---|
| Peak Time (hours) | 1.5-3 | 2-4 | 1-2 | 1-2 |
| Half-Life (hours) | ~11 | 6-9 | 13 | 2 (parent) |
| Active Metabolite? | No | No | No | Yes (EXP3174) |
| Food Effect | Slows absorption, no reduction | Reduces absorption by 30% | Minimal effect | Minimal effect |
| Primary Excretion | Kidneys (60%), Feces (40%) | Feces (70%), Kidneys (30%) | Feces (60%), Kidneys (40%) | Kidneys (65%), Feces (35%) |
| Typical Daily Dose | 40-80 mg | 80-320 mg | 20-40 mg | 50-100 mg |
Azilsartan stands out for its combination of rapid absorption, long receptor binding, and minimal reliance on metabolism. It’s not the strongest in every category - olmesartan has a longer half-life - but it’s the most consistent in delivering 24-hour control with once-daily dosing.
Is azilsartan safe for long-term use?
Yes. Azilsartan has been studied in clinical trials lasting up to two years, and long-term use is well tolerated. No new safety signals have emerged with extended use. It’s approved for lifelong management of hypertension, especially in patients with diabetes or kidney disease where protecting the kidneys matters.
Can I take azilsartan if I have kidney problems?
Most people with mild to moderate kidney disease can take azilsartan without dose changes. If your eGFR is below 30 mL/min, your doctor may reduce the dose or monitor you more closely. It’s not removed by dialysis, so it’s safe for patients on hemodialysis. Always get your kidney function checked before starting and periodically after.
Does azilsartan cause cough like ACE inhibitors?
No. Unlike ACE inhibitors (like lisinopril), azilsartan does not cause a dry cough. That’s because it blocks angiotensin II receptors directly, not the enzyme that produces it. This makes it a preferred alternative for people who can’t tolerate ACE inhibitors due to cough.
How soon does azilsartan start working?
You may see a drop in blood pressure within 1-2 weeks, but full effect takes about 4-6 weeks. Don’t expect immediate results. The goal is steady, long-term control, not a quick fix. Keep taking it even if you feel fine.
Can azilsartan be taken with other blood pressure meds?
Yes. Azilsartan is often combined with diuretics (like chlorthalidone), calcium channel blockers (like amlodipine), or even low-dose beta-blockers. These combinations are common and effective. Avoid combining it with other ARBs or ACE inhibitors - that increases risk of kidney injury and high potassium without added benefit.


Tyler Wolfe
took mine with breakfast and didn’t notice any delay. maybe i’m just lucky.