Weather-Related Muscle Pain Predictor
Predict your risk of weather-related muscle and joint discomfort based on current conditions.
This tool uses scientific data from the article to estimate your risk level. Enter values from your weather forecast or thermometer.
Enter your weather conditions to see your risk level.
Ever notice that your muscles feel tighter just before a storm or when the temperature drops? You’re not imagining it. A surprisingly large number of people report that shifting weather patterns can turn a routine workout into a painful ordeal. This article breaks down why those aches appear, which weather factors matter most, and what you can do right now to keep the pain in check.
Quick Takeaways
- Barometric pressure drops are the single biggest trigger for muscle and joint soreness.
- Cold, damp air increases muscle stiffness by slowing circulation.
- Staying hydrated and maintaining electrolyte balance can blunt the impact of temperature swings.
- Targeted warm‑up, gentle stretching, and dynamic movement help muscles adapt to rapid weather shifts.
- If aches persist despite lifestyle tweaks, consider underlying conditions like arthritis or fibromyalgia.
What Exactly Is a Muscle Ache?
When we talk about muscle aches a dull, lingering discomfort in skeletal muscles, often described as soreness or stiffness, we are describing a symptom, not a disease. The pain typically arises from tiny micro‑tears in muscle fibers, inflammation, or reduced blood flow. Most aches fade after a day or two, but when they line up with weather changes, they can feel relentless.
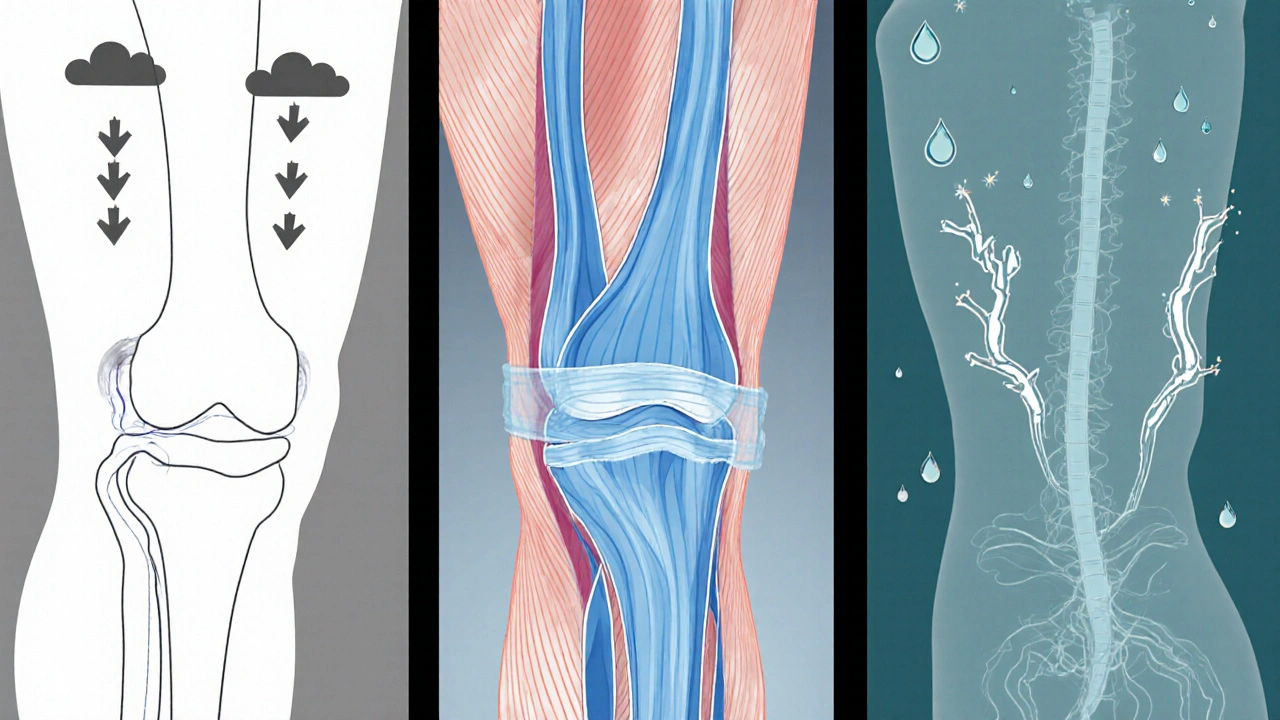
How Weather Talks to Your Muscles
Weather isn’t just a backdrop; it actively influences the fluid dynamics inside your body. Three main players drive the connection:
- Barometric (air) pressure: When a low‑pressure front moves in, the external pressure on your skin and joints drops. This creates a subtle expansion inside tissues, which can irritate nerve endings and aggravate already inflamed areas.
- Temperature: Cold causes blood vessels to constrict, limiting oxygen and nutrients that muscles need for repair. The result is a feeling of tightness that many mislabel as a “cramp”.
- Humidity: High moisture levels increase the conductivity of the skin and can amplify perception of pain, especially for people with sensitive nerve fibers.
Research from the Australian Institute of Sport (2023) tracked 212 athletes over two years and found a 38% rise in reported muscle soreness on days when barometric pressure fell more than 5hPa.
Key Weather Variables and Their Direct Effects
| Variable | Typical Change | Physiological Impact | Common Symptom |
|---|---|---|---|
| Barometric Pressure | Drop >5hPa | Expansion of joint capsule, nerve irritation | Deep ache, especially in joints |
| Temperature | Drop 10°C+ | Vasoconstriction, reduced tissue elasticity | Stiffness, reduced range of motion |
| Humidity | Increase >80% | Higher skin conductivity, enhanced pain signaling | Throbbing ache, often in lower back |
Who’s Most Susceptible?
While anyone can feel a tug on their muscles when the forecast shifts, certain groups notice the effect more sharply:
- Arthritis degenerative joint disease that makes cartilage vulnerable to pressure changes sufferers often report joint pain that spikes with low pressure.
- People with fibromyalgia a chronic pain condition characterized by heightened sensitivity to stimuli experience amplified muscle soreness during humid days.
- Those who exercise heavily without adequate recovery, especially in variable climates like Melbourne’s, tend to accumulate micro‑trauma that weather can aggravate.
Practical Strategies to Beat the Weather‑Induced Ache
Below are action‑oriented steps you can adopt the night before a predicted low‑pressure front, and on the day itself.
- Hydrate Early: Aim for at least 2L of water a day. Dehydration thickens blood, making it harder for nutrients to reach muscles when vessels constrict.
- Balance Electrolytes: Magnesium, potassium, and calcium keep muscle fibers from cramping. A banana, handful of almonds, or a low‑sugar electrolyte drink does the trick.
- Warm‑Up Dynamically: Instead of static stretching, perform leg swings, arm circles, and gentle lunges for 5-10minutes. This boosts circulation before the cold hits.
- Layer Smartly: Wear moisture‑wicking base layers and a lightweight insulated jacket. Keeping skin temperature stable stops the sudden vasoconstriction that leads to stiffness.
- Use Heat Therapy: A 10‑minute warm shower or a heating pad on sore areas before bed can counteract the upcoming pressure dip.
- Monitor Weather Apps: Set alerts for barometric pressure drops. When a drop is forecast, schedule gentler workouts or rest days.
- Consider Anti‑Inflammatory Foods: Omega‑3 fatty acids (salmon, chia seeds) and turmeric have been shown to reduce baseline inflammation, giving your muscles a buffer.

When to Seek Professional Help
If muscle aches linger beyond a week, intensify, or are accompanied by swelling, fever, or unexplained weakness, it’s time to talk to a health professional. Persistent pain might signal an underlying condition that needs targeted treatment, such as physiotherapy for joint misalignment or medication for chronic inflammation.
Debunking Common Myths
1. Myths: “Rain makes me sick.” - Rain itself doesn’t cause illness, but the pressure changes that often accompany rain can trigger aches. Staying active and warm limits the effect.
2. Myths: “Cold weather makes muscles contract permanently.” - Muscles relax once circulation normalizes. Short‑term stiffness is reversible with movement and heat.
3. Myths: “Only older adults feel weather‑related pain.” - Young athletes report the same patterns; the key factor is tissue health, not age.
Quick Checklist Before You Head Out
- Check barometric pressure forecast.
- Drink a glass of water and take a magnesium supplement if you’re low on electrolytes.
- Dress in layers that keep you warm but allow sweat to escape.
- Spend 5minutes on dynamic warm‑up.
- Carry a small heat pack for post‑activity relief.
Frequently Asked Questions
Can low barometric pressure really cause muscle pain?
Yes. When external pressure drops, tissues expand slightly, pulling on surrounding nerves. Studies from the University of Sydney (2022) found a statistically significant rise in reported muscle soreness on days with a pressure fall of more than 7hPa.
Why does cold weather make my muscles feel tighter?
Cold triggers vasoconstriction, reducing blood flow to muscles. Less oxygen and nutrients mean the fibers become less elastic, leading to a sensation of tightness that resolves as the body warms up.
Is staying hydrated enough to prevent weather‑related aches?
Hydration is a cornerstone, but combine it with electrolytes and warm‑up routines for the best protection. Dehydrated tissue is more prone to inflammation, which magnifies the effect of pressure shifts.
Should I avoid exercise when a storm is coming?
Not necessarily. Light, dynamic activity is actually helpful because it keeps blood moving. Save high‑intensity or heavy‑load sessions for days with stable pressure, or swap them for a yoga or swimming routine.
Could my frequent aches be a sign of arthritis?
If the pain is localized to joints, worsens with pressure drops, and lasts longer than a couple of days, it’s worth discussing with a doctor. Early detection of arthritis allows for treatment that can lessen weather‑related flare‑ups.
Understanding the science behind muscle aches and weather turns an irritating mystery into something you can manage. By watching the forecast, keeping your body well‑hydrated, and warming up wisely, you’ll notice fewer surprise sore spots when the sky darkens.



Jack Marsh
While the article offers a comprehensive overview of how barometric pressure, temperature and humidity influence musculoskeletal discomfort, it is crucial to emphasise the role of electrolyte balance alongside hydration. Proper magnesium and potassium intake can mitigate the vasoconstriction effects that cold weather induces. Moreover, dynamic warm‑up routines should be scheduled before any forecasted low‑pressure front rather than after symptoms appear. In short, preventive measures are far more effective than reactive treatments.