Ulcerative colitis isn’t just frequent bathroom trips or cramps. It’s a chronic condition where your colon’s inner lining becomes inflamed, develops open sores, and doesn’t heal on its own. Unlike a stomach bug that fades in a few days, ulcerative colitis (UC) comes and goes in unpredictable waves - sometimes quiet for months, other times flaring with bloody diarrhea, severe pain, and exhaustion. If you’ve been diagnosed or suspect you might have it, you’re not alone. About 1 in 200 people in Australia live with this condition, and most of them find ways to manage it - not just survive, but live full lives.
What Exactly Happens in Your Colon?
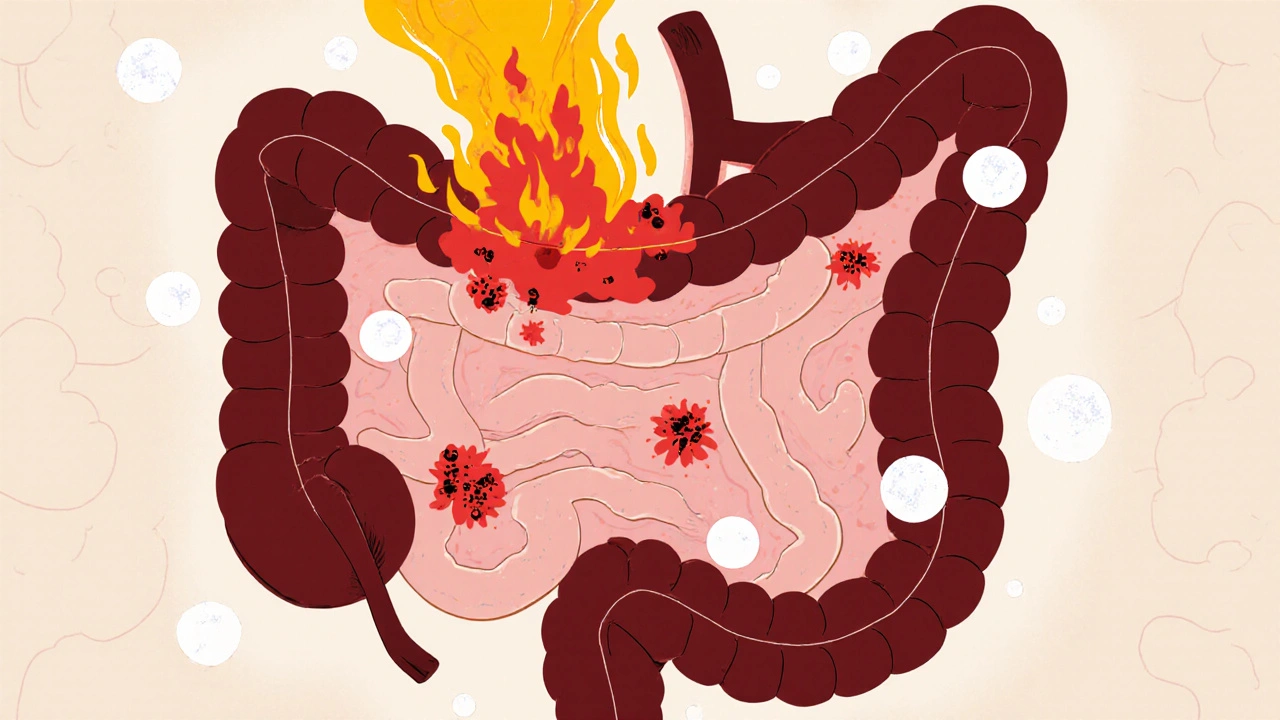
Ulcerative colitis attacks only the large intestine - the colon and rectum. It doesn’t jump around like Crohn’s disease. Instead, it starts in the rectum and spreads upward in a continuous line, like a slow-burning fuse. The inflammation doesn’t just make things red and swollen; it eats away at the top layer of tissue, creating ulcers. These aren’t like skin sores - they’re deep, raw patches that bleed and leak mucus, which is why bloody stool is the #1 sign of UC.
There are five main types, based on how far up the colon the inflammation reaches:
- Ulcerative proctitis: Only the rectum is affected. Symptoms are usually mild - occasional bleeding, urgency, maybe some discomfort.
- Proctosigmoiditis: Inflammation reaches the sigmoid colon (the lower S-shaped part). More frequent bowel movements, cramps on the left side.
- Left-sided colitis: Goes as far as the splenic flexure (near the spleen). You’ll feel pain on your left side, lose weight, and have more than 10 bowel movements a day.
- Pancolitis: The entire colon is inflamed. This is the most severe form - constant bloody diarrhea, fever, fatigue, and major weight loss.
- Rectal-sparing UC: Rare. The rectum stays healthy, but everything above it is damaged.
The pattern matters. If your inflammation is patchy - healthy tissue between inflamed spots - it’s probably not UC. That’s Crohn’s disease. UC doesn’t skip. It’s all or nothing along the colon’s lining.
Why Does This Happen?
No one knows exactly why your immune system turns on your own colon. But we know it’s not your fault. You didn’t eat too much junk food. You didn’t stress too hard. Those things don’t cause UC - but they can trigger a flare.
The leading theory is autoimmune. Your body’s defense system gets confused. It thinks the lining of your colon is a threat, so it sends white blood cells to attack. The result? Swelling, ulcers, and pain. Genetics play a role too. If a close family member has UC or another autoimmune disease like psoriasis or rheumatoid arthritis, your risk goes up. People of Ashkenazi Jewish descent are also at higher risk.
Age is another factor. Two peaks show up: one in your teens and twenties, another in your fifties and sixties. That means UC can hit when you’re starting college or when you’re nearing retirement. Neither is easy to manage.
What Does a Flare Feel Like?
Flares don’t come with warning signs. One day you’re fine. The next, you’re racing to the bathroom every 20 minutes. Here’s what’s common:
- Bloody diarrhea: Happens in nearly every case. Stool might be watery, streaked with blood, or look like pus.
- Tenesmus: That awful feeling you need to go - even when your bowels are empty. It’s like your colon is screaming for help.
- Abdominal cramps: Usually on the left side, but can be all over. Pain doesn’t go away with passing stool.
- Urgency: You can’t wait. Even a short car ride becomes a nightmare.
- Fatigue and fever: Your body is fighting a constant internal battle. You’re drained, even after sleeping.
- Weight loss and poor appetite: When your gut hurts, eating feels impossible. Calories vanish fast.
Some people also get symptoms outside the gut. Joint pain, red or itchy eyes, skin rashes - these are called extraintestinal manifestations. They’re not random. They’re part of the same immune system malfunction.
How Do You Get Into Remission?
Remission doesn’t mean cured. It means the inflammation has quieted down. No blood in stool. No pain. No urgency. You can go back to work, travel, sleep through the night. And yes - it’s possible.
Medication is the backbone of remission. Treatment follows a step-by-step approach:
- 5-ASAs (mesalamine, sulfasalazine): First-line for mild to moderate UC. These drugs reduce inflammation right where it’s happening. They come as pills, suppositories, or enemas. If your disease is only in the rectum, an enema can be more effective than a pill.
- Corticosteroids: Used short-term during flares. They work fast - but can’t be used long-term because of side effects like bone loss, weight gain, and mood swings.
- Immunomodulators: Drugs like azathioprine or 6-MP. These calm the immune system over time. Takes 3-6 months to kick in. Used when 5-ASAs aren’t enough.
- Biologics: Newer, targeted drugs like infliximab, adalimumab, vedolizumab. They block specific proteins in the immune response. Many people with moderate to severe UC go into deep remission with these. Some stay in remission for years.
Surgery - removing the colon - is the only true cure. But it’s not the first option. It’s reserved for people who don’t respond to meds, have dangerous complications, or have a high cancer risk from long-standing pancolitis.
What About Diet and Lifestyle?
Diet doesn’t cause UC. But what you eat can make flares worse or better. During a flare, high-fiber foods like raw veggies, nuts, and whole grains can irritate your gut. Dairy might cause bloating if you’re lactose intolerant - common in UC. Spicy foods, caffeine, and alcohol are common triggers too.
Keep a food diary. Write down what you eat and how you feel. You’ll start seeing patterns. Maybe tomatoes trigger you. Or maybe chocolate is fine. Everyone’s different.
Stress won’t cause UC, but it can make flares more likely. You don’t need to live in a bubble. But learning to manage stress - through yoga, walking, therapy, or meditation - helps. Sleep matters too. Poor sleep = more inflammation.
Hydration is critical. Diarrhea steals fluids and electrolytes. Drink water. Consider oral rehydration solutions if you’re losing a lot.

Monitoring and Long-Term Risks
Even when you’re in remission, you still need check-ups. The biggest long-term risk? Colon cancer. The longer you have UC - especially if it affects your whole colon - the higher your risk. That’s why regular colonoscopies are non-negotiable.
Doctors recommend your first colonoscopy 8 years after diagnosis, then every 1-2 years after that. They look for dysplasia - abnormal cell changes that can turn into cancer. Catching it early means you can remove the affected area before it spreads.
Other risks include severe bleeding, toxic megacolon (a dangerous swelling of the colon), and perforation. These are rare, but they need emergency care. Know the warning signs: sudden severe pain, high fever, rapid heartbeat. Don’t wait.
You Can Still Live Well
People with UC don’t have to give up their lives. Many run marathons. Raise kids. Travel overseas. Work full-time. The key? Finding the right treatment and sticking with it.
Modern medicine has changed everything. Ten years ago, biologics weren’t widely available. Now, they’re helping people stay in remission for years. Clinical trials are testing even more targeted drugs with fewer side effects.
Join a support group. Talk to others who get it. You don’t have to explain the urgency, the fear, the exhaustion. They already know.
Remission isn’t a finish line. It’s a daily practice - taking your meds, listening to your body, managing stress, and staying on top of screenings. But it’s absolutely within reach.
Can ulcerative colitis be cured without surgery?
There’s no medical cure for ulcerative colitis - medications can’t permanently fix the immune system’s mistake. But many people achieve long-term remission without surgery. With the right combination of 5-ASAs, immunomodulators, or biologics, inflammation can stay under control for years. Surgery to remove the colon is the only way to eliminate the disease completely, but it’s not required for most people.
Does stress cause ulcerative colitis?
No, stress doesn’t cause ulcerative colitis. The root cause is an overactive immune response, likely tied to genetics and environmental triggers. But stress can make symptoms worse and trigger flares. Managing stress through sleep, exercise, or therapy helps reduce flare frequency - not because it cures UC, but because it lowers the body’s overall inflammatory load.
Can I drink alcohol with ulcerative colitis?
Alcohol can irritate the gut lining and worsen diarrhea, cramping, and urgency - especially during a flare. While some people tolerate small amounts when in remission, many find that even one drink triggers symptoms. It’s best to avoid alcohol during flares and limit it when you’re stable. If you do drink, stick to low-sugar, low-alcohol options and monitor how you feel.
Is ulcerative colitis the same as IBS?
No. IBS (irritable bowel syndrome) is a functional disorder - meaning the gut looks normal but doesn’t work right. UC is an inflammatory disease with visible ulcers, bleeding, and tissue damage. IBS doesn’t increase cancer risk or require biologics. UC can lead to hospitalization and surgery. They share symptoms like diarrhea and cramps, but the causes and treatments are completely different.
How often do I need a colonoscopy?
If you’ve had UC for 8 years or more, especially if it affects your whole colon (pancolitis), you should have a colonoscopy every 1-2 years to screen for dysplasia and early cancer. If your disease is limited to the rectum (proctitis), your risk is much lower, and screening may be less frequent. Your gastroenterologist will tailor the schedule based on your disease extent, duration, and family history.
Can children get ulcerative colitis?
Yes. About 25% of UC cases are diagnosed before age 20. Pediatric UC can be more aggressive and affect growth and development. Treatment is similar to adults but carefully adjusted for weight and age. Early diagnosis and treatment are critical to prevent complications and help kids thrive in school and social settings.
What happens if I stop taking my medication?
Stopping medication is the most common reason for flare-ups. Even if you feel fine, the inflammation may still be there under the surface. Stopping 5-ASAs or biologics suddenly can cause your immune system to rebound aggressively. Always talk to your doctor before making changes. Sometimes, doses can be lowered slowly - but never stopped without medical guidance.
What’s Next?
If you’re newly diagnosed, give yourself time. It’s overwhelming. But you’re not alone. Work with a gastroenterologist who specializes in IBD. Find a dietitian who understands UC. Connect with others through support groups - online or in person.
If you’ve had UC for years and are struggling to stay in remission, it’s time to revisit your treatment plan. Biologics have improved dramatically. New oral drugs like JAK inhibitors are now available and might be an option if your current meds aren’t working.
Remission isn’t magic. It’s science. It’s consistency. It’s listening to your body - and trusting the process. You can live well with ulcerative colitis. You just need the right tools, and the patience to use them.


Peter Aultman
Been living with UC for 12 years. Took me 5 tries to find the right med combo, but now I’m in deep remission. No blood, no urgency, even drank a beer last weekend. It’s not perfect, but it’s life.
Just keep going. You got this.