Understanding Chronic Lymphocytic Leukemia
Chronic Lymphocytic Leukemia (CLL) is a type of blood cancer that affects the white blood cells known as lymphocytes. In CLL, the body produces an excessive number of abnormal, immature lymphocytes that accumulate in the blood and bone marrow, crowding out healthy cells and impairing the immune system. The disease is slow-growing, and many people may not experience symptoms for several years. However, as the disease progresses, symptoms such as fatigue, enlarged lymph nodes, and infections become more prominent, necessitating treatment.
Traditional treatment options for CLL have included chemotherapy, radiation therapy, and stem cell transplants. While these treatments can be effective, they also come with significant side effects and may not be suitable for all patients. In recent years, targeted therapies have emerged as a promising new approach to treating CLL, offering the potential for improved outcomes and fewer side effects.
The Importance of Targeted Therapy
Targeted therapies are a new class of cancer treatments that work by specifically targeting the underlying molecular abnormalities that drive cancer growth and survival. Unlike traditional chemotherapy, which affects both cancerous and healthy cells, targeted therapies are designed to act on cancer cells while sparing normal cells. This more precise approach can lead to fewer side effects and better outcomes for patients.
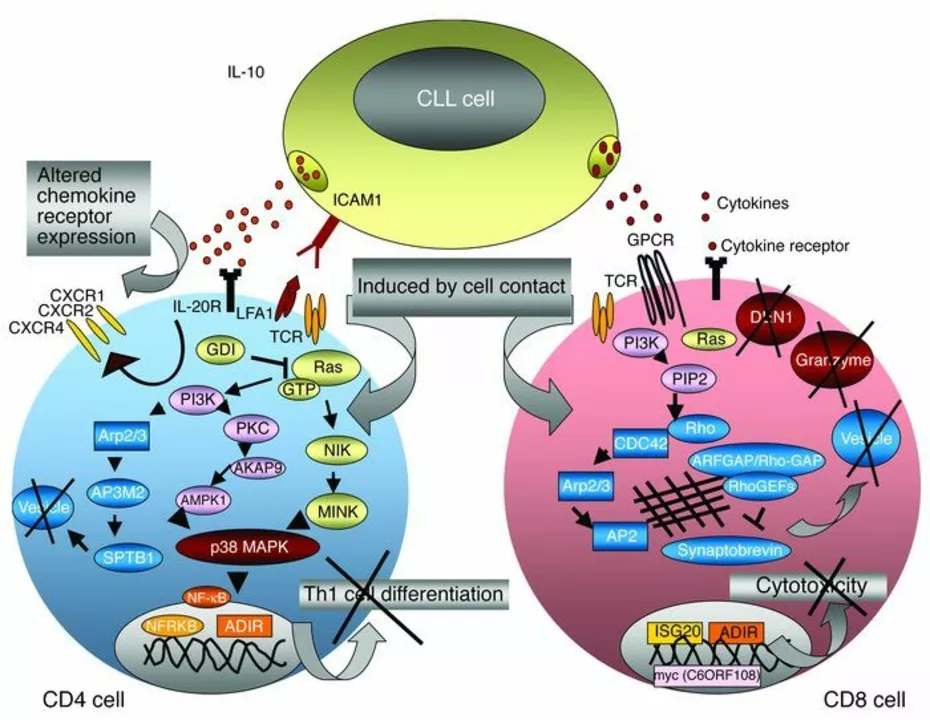
In CLL, researchers have identified several key molecular pathways that play a role in the development and progression of the disease. By developing drugs that target these specific pathways, scientists hope to create more effective treatments with fewer side effects.
Breaking Down B-cell Receptor Signaling
One of the most promising targets in CLL is the B-cell receptor (BCR) signaling pathway. BCR signaling is essential for the survival and proliferation of normal B-cells, but it is also hijacked by CLL cells to promote their growth and survival. Several targeted therapies have been developed to disrupt BCR signaling, including ibrutinib, idelalisib, and duvelisib.
Ibrutinib is a first-in-class drug that works by irreversibly inhibiting a key enzyme called Bruton's tyrosine kinase (BTK) in the BCR signaling pathway. By blocking BTK, ibrutinib can halt the growth and survival signals that drive CLL cells, leading to cell death. This targeted approach has shown significant success in clinical trials, with ibrutinib demonstrating improved response rates and overall survival compared to traditional chemotherapy.
Targeting Abnormal Cell Survival
Another key target in CLL is the BCL-2 protein, which plays a critical role in regulating cell survival and is overexpressed in many CLL cells. Venetoclax is a targeted therapy that works by binding to BCL-2 and selectively blocking its function, thereby promoting the death of CLL cells. Clinical trials have shown that venetoclax is highly effective in treating CLL, particularly in patients who have relapsed or are resistant to other therapies.
Combination therapies that include venetoclax and other targeted agents, such as ibrutinib or obinutuzumab, are also being explored in clinical trials, with promising results thus far.
Overcoming Resistance to Targeted Therapies
While targeted therapies have shown great promise in the treatment of CLL, resistance to these drugs can still occur. In some cases, CLL cells may develop genetic mutations that allow them to evade the effects of targeted therapies, leading to disease progression. Understanding the mechanisms of resistance is a crucial area of ongoing research, as it can inform the development of new drugs and combination strategies to overcome resistance and improve patient outcomes.
One example of a drug developed to overcome resistance is acalabrutinib, a second-generation BTK inhibitor. This drug is designed to be more selective and potent than ibrutinib, potentially overcoming resistance and providing a new treatment option for patients who have failed other therapies.
Personalizing Treatment for CLL Patients
As our understanding of the molecular basis of CLL continues to grow, so does the potential for personalized medicine. By identifying the specific genetic abnormalities driving a patient's disease, clinicians can select the most appropriate targeted therapy, improving the chances of a successful outcome.
This personalized approach to treatment is already being used in some cases, with the testing of certain genetic markers now recommended as part of the standard workup for CLL patients. As more targeted therapies become available, it is likely that this approach will become increasingly common and essential in the management of CLL.
Looking to the Future: Immunotherapy and Beyond
While targeted therapies have already made a significant impact on the treatment landscape for CLL, there is still much work to be done. Researchers continue to investigate new targets, and the potential for combination therapies and personalized medicine is vast. Additionally, immunotherapy – a type of treatment that harnesses the patient's immune system to fight cancer – is an emerging area of interest in CLL research.
One type of immunotherapy being explored for CLL is chimeric antigen receptor (CAR) T-cell therapy, in which a patient's own immune cells are genetically engineered to recognize and attack cancer cells. Early results from clinical trials of CAR T-cell therapy in CLL have been promising, and further research is ongoing.
Overall, the future of CLL treatment appears bright, with targeted therapies paving the way for more effective, less toxic treatment options. As we continue to unlock the molecular secrets of this disease, the hope is that one day we will be able to provide a cure for all CLL patients.


Prema Amrita
Ibrutinib changed my father's life. No more hospital visits every other week. Just a pill and he's out gardening. The side effects? Barely there. I wish we had this ten years ago.
Thank you for writing this.