Antiviral Selection Tool
Personalized Antiviral Recommendation
Select your patient's characteristics to receive a recommendation based on the latest clinical evidence.
Select patient characteristics to see a personalized recommendation.
Key Takeaways
- Molnupiravir is an oral antiviral that reduces hospitalization by ~30% in high‑risk patients.
- Paxlovid (nirmatrelvir+ritonavir) shows the highest reduction (~89%) but has many drug‑interaction warnings.
- Remdesivir is given intravenously, useful for hospitalized cases, with a 5‑day course cutting recovery time.
- Favipiravir offers modest benefit and is mainly used where other options are unavailable.
- Choosing the right drug depends on timing of infection, patient comorbidities, and access to healthcare facilities.
When treating COVID‑19, Molnupiravir is an oral antiviral that introduces copying errors into the SARS‑CoV‑2 genome, halting viral replication. Since its emergency use authorization in early 2022, doctors have asked how it stacks up against other antivirals. This guide walks through the science, the real‑world numbers, and the practical pros and cons so you can decide which option fits a given patient best.
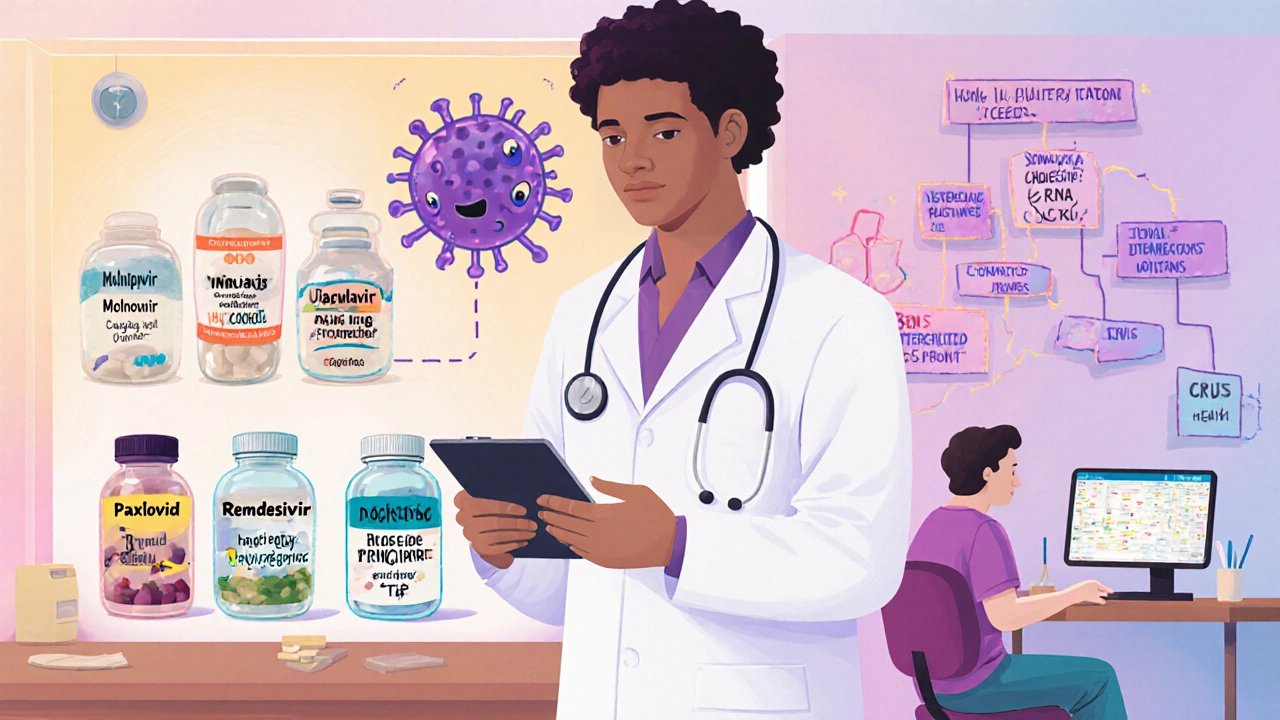
Understanding the Players
Paxlovid is a combination of nirmatrelvir (a protease inhibitor) and ritonavir (a pharmacokinetic booster) taken orally for five days. Clinical trials published in the New England Journal of Medicine showed an 89% drop in hospitalization risk when started within three days of symptom onset.
Remdesivir is an intravenous nucleoside analog that stalls the viral RNA‑dependent RNA polymerase. The ACTT‑1 trial demonstrated a 5‑day course shortened median recovery time from 15 to 10 days in hospitalized patients.
Favipiravir is a broad‑spectrum oral polymerase inhibitor originally approved for influenza in Japan. Its COVID‑19 data are mixed, but some real‑world registries report a 15‑20% reduction in progression when given early.
Lagevrio is the brand name under which Molnupiravir is marketed in the United States and Europe. The formulation is identical; the name is useful for pharmacy‑level discussions.
The virus itself matters. SARS‑CoV‑2 is the coronavirus responsible for the COVID‑19 pandemic. Its rapid mutation rate creates new variants that can shift drug effectiveness, a factor we’ll revisit.
How Each Drug Works
- Molnupiravir/Lagevrio: Incorporates as a ribonucleoside analogue, causing “error catastrophe” in viral RNA.
- Paxlovid: Blocks the main protease (Mpro), preventing the virus from processing essential proteins.
- Remdesivir: Mimics adenosine, causing premature termination of the RNA chain.
- Favipiravir: Acts as a purine analogue, inhibiting the RNA‑dependent RNA polymerase.
All four target the replication step, but their delivery methods and resistance profiles differ. Oral pills (Molnupiravir, Paxlovid, Favipiravir) are convenient for early outpatient care, while Remdesivir requires a clinic or hospital infusion.
Clinical Efficacy at a Glance
| Drug | Mechanism | Administration | Hospitalization Reduction* | Approval (US/EU) | Key Side Effects |
|---|---|---|---|---|---|
| Molnupiravir | RNA error‑inducing nucleoside analogue | Oral, 800mg BID for 5days | ≈30% (pre‑Omicron data) | Emergency Use Authorization (US), Conditional (EU) | Nausea, dizziness, rare mutagenicity concerns |
| Paxlovid | Protease inhibition (nirmatrelvir) + CYP3A4 boost (ritonavir) | Oral, 300mg/100mg BID for 5days | ≈89% (EPIC‑HR trial) | Full FDA approval (US), Conditional (EU) | Altered taste, diarrhea, many drug interactions |
| Remdesivir | \nChain‑terminating nucleoside analogue | IV infusion 200mg day1 then 100mg daily (5days) | ≈30% reduction in time to recovery | Full FDA approval (US), EMA approval (EU) | Elevated liver enzymes, infusion‑related reactions |
| Favipiravir | Polymerase inhibition (purine analogue) | Oral, 1800mg BID loading then 800mg BID (5‑7days) | ≈15‑20% (observational studies) | Approved for influenza in Japan; off‑label for COVID‑19 | Hyperuricemia, teratogenic risk |
*Hospitalization reduction percentages are derived from pivotal phaseIII trials and may vary with circulating variants.
When to Choose Each Option
- Early outpatient (≤5days from symptom onset) with high‑risk comorbidities: Paxlovid is the first‑line choice if no contraindicated drug interactions exist. Molnupiravir is a good fallback when ritonavir‑based regimens are unsafe.
- Patients on multiple medications (e.g., statins, anticoagulants): Molnupiravir’s low interaction profile makes it attractive, despite its lower efficacy.
- Hospitalized or requiring supplemental oxygen: Remdesivir remains the only IV antiviral with solid evidence for shortening recovery.
- Resource‑limited settings where Paxlovid is unavailable: Favipiravir or Molnupiravir can be sourced locally, provided dosing oversight.
Safety Nuances You Can’t Ignore
The biggest controversy around Molnupiravir is its mutagenic potential. In vitro assays flagged possible DNA incorporation, but animal studies at therapeutic doses showed no significant genotoxicity. Regulatory agencies therefore limit use to patients 18years and older with a clear risk‑benefit justification.
Paxlovid’s ritonavir component is a potent CYP3A4 inhibitor. That means drugs like certain anti‑arrhythmics, immunosuppressants, and some anticonvulsants may reach toxic levels. Clinicians must review medication lists thoroughly-often using a clinical decision support tool.
Remdesivir requires baseline liver‑function testing and monitoring of renal function (eGFR≥30mL/min). Its IV nature can cause phlebitis or hypersensitivity reactions, so infusion centers need trained staff.
Favipiravir is teratogenic in animal models; women of child‑bearing potential must use effective contraception during treatment and for at least a month afterward.
Cost and Availability in 2025
In the United States, a full Paxlovid course costs about U.S. Department of Health and Human Services funding for eligible patients, making it effectively free. Molnupiravir’s price, after negotiations, sits around $500 for the 5‑day pack.
In Australia, both Paxlovid and Molnupiravir are listed on the Pharmaceutical Benefits Scheme (PBS), but supply constraints occasionally prioritize Paxlovid for the highest‑risk groups. Remdesivir is reimbursed for inpatient use, and Favipiravir is imported on a case‑by‑case basis.
Putting It All Together: Decision Tree
Below is a quick mental checklist you can follow during a telehealth visit:
- Is the patient within 5 days of symptom onset? If no, consider supportive care or hospital referral.
- Does the patient take medications that interact with ritonavir? If yes, skip Paxlovid.
- Are they pregnant, trying to conceive, or under 18? Avoid Molnupiravir and Favipiravir.
- Can the patient receive an IV infusion? If yes and already hospitalized, choose Remdesivir.
- Otherwise, weigh efficacy vs. safety: Paxlovid > Molnupiravir > Favipiravir.
Future Outlook
New antivirals like ensitrelvir (Xocova) received EMA approval in early 2024, showing 88% efficacy against Omicron sub‑variants. While not yet widely available in the U.S., they signal a shift toward more potent oral options that may eventually dethrone Paxlovid.
Additionally, ongoing surveillance by the World Health Organization (WHO) suggests that combination therapy (e.g., Paxlovid+Molnupiravir) could reduce resistance emergence, though trials are still enrolling.
Bottom Line
If you need the highest efficacy and can manage drug‑interaction checks, Paxlovid stays the top pick. Molnupiravir offers a simpler safety profile for patients on many meds, but expect a modest benefit. Remdesivir remains the go‑to for hospitalized cases, and Favipiravir is a fallback where other drugs are scarce. Always align the choice with timing, comorbidities, and local availability.
Frequently Asked Questions
Can I take Molnupiravir and Paxlovid together?
Current guidance advises against simultaneous use because both target viral replication and may increase side‑effect risk without proven added benefit. Choose one based on the patient’s drug‑interaction profile.
How soon after exposure should I start an antiviral?
The earlier, the better. All oral antivirals (Molnupiravir, Paxlovid, Favipiravir) show the greatest reduction in severe outcomes when started within 3-5 days of symptom onset.
Is Molnupiravir safe for people with kidney disease?
Molnupiravir is primarily cleared by the liver, so mild to moderate renal impairment does not require dose adjustment. Severe renal failure (eGFR<15mL/min) should be evaluated case‑by‑case.
What are the most common side effects of Paxlovid?
Patients often report a bitter or metallic taste, diarrhea, and mild hypertension. The biggest concern is drug‑drug interactions due to ritonavir’s CYP3A4 inhibition.
Do I need a prescription for Favipiravir?
Yes. In most countries it is a prescription‑only medication, often limited to clinical trial or compassionate‑use programs for COVID‑19.


Darryl Gates
Thanks for pulling all that data together; it really helps clinicians make quick decisions. I especially like the clear checklist at the end – it’s exactly what busy doctors need in a telehealth visit. The distinction between oral and IV options is spot‑on, and the side‑effect notes are concise. For anyone juggling drug interactions, the Paxlovid warning section is a lifesaver.