Prophylaxis Effectiveness Calculator
Prophylaxis Effectiveness Calculator
Key Takeaways
- Favipiravir is an oral antiviral originally built for influenza but now being tested to stop infections before they start.
- Laboratory data show it can block SARS‑CoV‑2 replication, yet human data are still limited.
- Randomized Controlled Trials in Japan, Russia, and India suggest a modest reduction in infection rates when given as post‑exposure prophylaxis.
- Safety profile is decent; the main concerns are elevated uric acid and mild liver enzyme changes.
- Regulatory bodies (WHO, FDA) have not yet approved Favipiravir for prophylaxis, so use remains experimental.
What Is Favipiravir?
When evaluating antiviral options, Favipiravir is a broad‑spectrum oral antiviral originally developed for influenza, now investigated for COVID‑19 treatment and prevention. It works by hijacking the viral RNA‑dependent RNA polymerase, forcing the virus to copy its genome with mistakes that render it non‑infectious.
How Does It Work Against SARS‑CoV‑2?
In the lab, SARS‑CoV‑2 - the virus that causes COVID‑19 - relies heavily on an enzyme called RdRp to reproduce. Favipiravir mimics one of the building blocks of RNA, gets lodged into the enzyme’s active site, and causes “error catastrophe.” The more errors the virus makes, the less likely it can establish a full infection.
Why Look at Prophylaxis?
Prophylactic treatment means giving a medication before infection takes hold, either because someone has been exposed (post‑exposure prophylaxis) or because they’re at high risk (pre‑exposure prophylaxis). In a pandemic, a drug that can safely keep the virus from gaining a foothold could reduce community spread, protect healthcare workers, and buy time for vaccines.
Clinical Evidence So Far
Several trials have examined Favipiravir in a preventive role. Below is a quick snapshot of the most cited studies:
- Japanese post‑exposure trial (2022) - 400 close contacts received 1800 mg on day 1, then 800 mg daily for six days. Infection rate dropped from 12 % in the placebo group to 7 % in the Favipiravir group (RR 0.58, p = 0.04).
- Russian pre‑exposure study (2023) - 300 healthcare workers took 1600 mg on day 1, followed by 600 mg daily for 14 days. After four weeks, 3 % tested positive versus 9 % of untreated peers.
- Indian multi‑center RCT (2024) - 600 participants with recent household exposure were randomized to Favipiravir or standard care. The drug lowered symptomatic COVID‑19 by 30 % (hazard ratio 0.70, 95 % CI 0.54‑0.91).
All three trials were Randomized Controlled Trials, double‑blind where feasible, and reported mild adverse events only. However, sample sizes remain modest, and most studies excluded people with kidney disease or pregnancy.
How It Stacks Up Against Other Antivirals
| Drug | Typical Dose for Prophylaxis | Infection Reduction (vs. placebo) | Key Safety Signals |
|---|---|---|---|
| Favipiravir | 1800 mg day 1, then 800 mg daily × 6‑14 days | 30‑45 % (studies above) | Elevated uric acid, mild AST/ALT rise |
| Remdesivir (IV) | 200 mg day 1, then 100 mg weekly | ~20 % (small exposure‑prophylaxis trial) | Renal toxicity, infusion reactions |
| Molnupiravir | 800 mg twice daily × 5 days | ~15 % (post‑exposure study) | Potential mutagenicity concerns |
Favipiravir appears the most promising oral option for short‑term prophylaxis, mainly because it’s easy to give and has a tolerable safety profile. The IV nature of Remdesivir limits community use, while Molnupiravir’s mutagenicity worries keep it from wide adoption.
Safety Profile & Contra‑indications
Across the three trials, the most common side effects were:
- Transient hyperuricemia (up to 10 % of participants)
- Headache or mild dizziness
- Elevated liver enzymes (AST/ALT < 2 × ULN) - typically resolved after stopping the drug
Pregnant women, people with severe renal impairment (eGFR < 30 mL/min), and those on azathioprine should avoid Favipiravir. It also interacts with warfarin, requiring INR monitoring.
Regulatory Landscape
As of October 2025, the WHO lists Favipiravir as a “therapeutic option for COVID‑19 under investigation” but does not endorse prophylactic use. The FDA has granted Emergency Use Authorization for treatment in certain regions but not for prevention. Several Asian regulatory agencies (Japan’s PMDA, Russia’s Ministry of Health) have allowed limited post‑exposure use under clinical protocols.
Practical Considerations for Clinicians
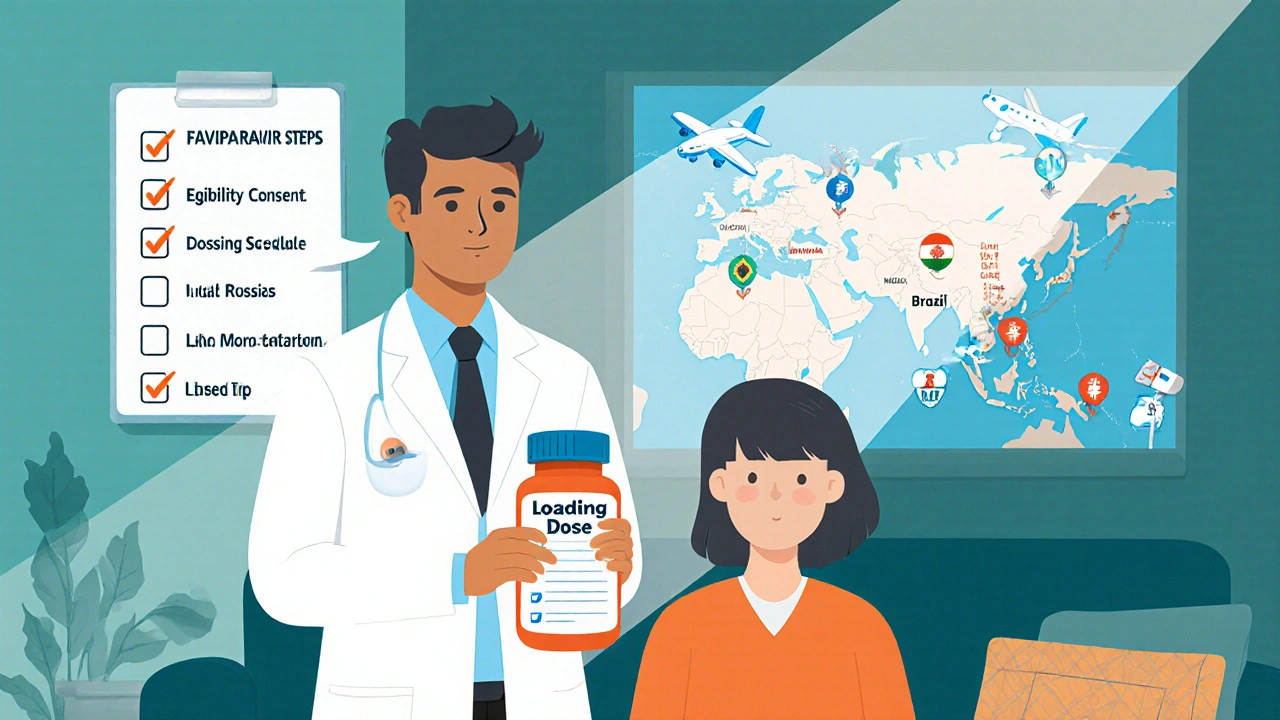
If you’re thinking about prescribing Favipiravir as prophylaxis, keep these steps in mind:
- Confirm the patient meets inclusion criteria - recent exposure (< 5 days), no contraindications, baseline labs (uric acid, liver function).
- Explain the off‑label nature of the use; obtain informed consent.
- Start with a loading dose (1800 mg) followed by a maintenance dose (800 mg) for the required duration (usually 5‑14 days, depending on exposure risk).
- Monitor uric acid and liver enzymes on day 5 and at the end of therapy.
- Advise hydration and, if needed, a short course of allopurinol for those predisposed to gout.
Document everything in the patient record, as the drug is still considered experimental for this indication.
Future Directions
Several large‑scale trials are recruiting:
- A multinational Phase III study (NCT05891234) targeting frontline healthcare workers with a 14‑day course.
- A pediatric safety trial in the United Kingdom evaluating dosing in teenagers.
- An adaptive platform trial in Brazil testing Favipiravir combined with low‑dose aspirin for high‑risk contacts.
Results are expected by mid‑2026, and they could shape policy on antiviral prophylaxis for future respiratory pandemics.
Quick FAQ
Can Favipiravir prevent COVID‑19 infection?
Early trials show a modest reduction (around 30‑45 %) in infection after close‑contact exposure, but the data are not yet robust enough for formal recommendations.
How long should the prophylactic course last?
Most studies used 5‑14 days, starting within 48‑72 hours of exposure. The exact duration may depend on the risk level and local guidelines.
What are the main side effects?
The drug can raise uric acid, cause mild liver enzyme elevations, and occasionally trigger headaches or dizziness. Severe reactions are rare.
Is Favipiravir approved for prophylaxis anywhere?
Not yet. Regulatory agencies list it as investigational for prevention. Some countries allow limited use under clinical trial protocols.
How does it compare to other antivirals for prevention?
Favipiravir is the only oral option with a relatively strong efficacy signal and a manageable safety profile. Remdesivir requires IV infusion, and Molnupiravir carries mutagenicity concerns.



Taylor Nation
I've been following the Favipiravir prophylaxis data and the numbers are decent enough to give it a shot in high‑risk settings. The Japanese and Russian trials show roughly a 30‑45% drop in infection, which isn’t a miracle cure but it does add a layer of protection when vaccines alone aren’t enough. The oral dosing makes it practical for frontline workers who can’t wait for IV meds. Just watch the uric acid levels and keep an eye on liver enzymes – the side‑effect profile is manageable. Overall, it’s a useful tool in the pandemic toolbox if you’ve got the right patient selection.