When eye drops and laser treatments stop controlling your eye pressure, surgery becomes the next step to protect your vision. Glaucoma doesn’t always cause symptoms until damage is done - that’s why lowering intraocular pressure (IOP) is the only proven way to slow or stop vision loss. Two main types of surgery are used today: traditional trabeculectomy and newer minimally invasive glaucoma surgery (MIGS). Each has clear strengths, risks, and ideal candidates. Knowing the difference helps you make smarter decisions with your eye doctor.
What Trabeculectomy Does and Who It’s For
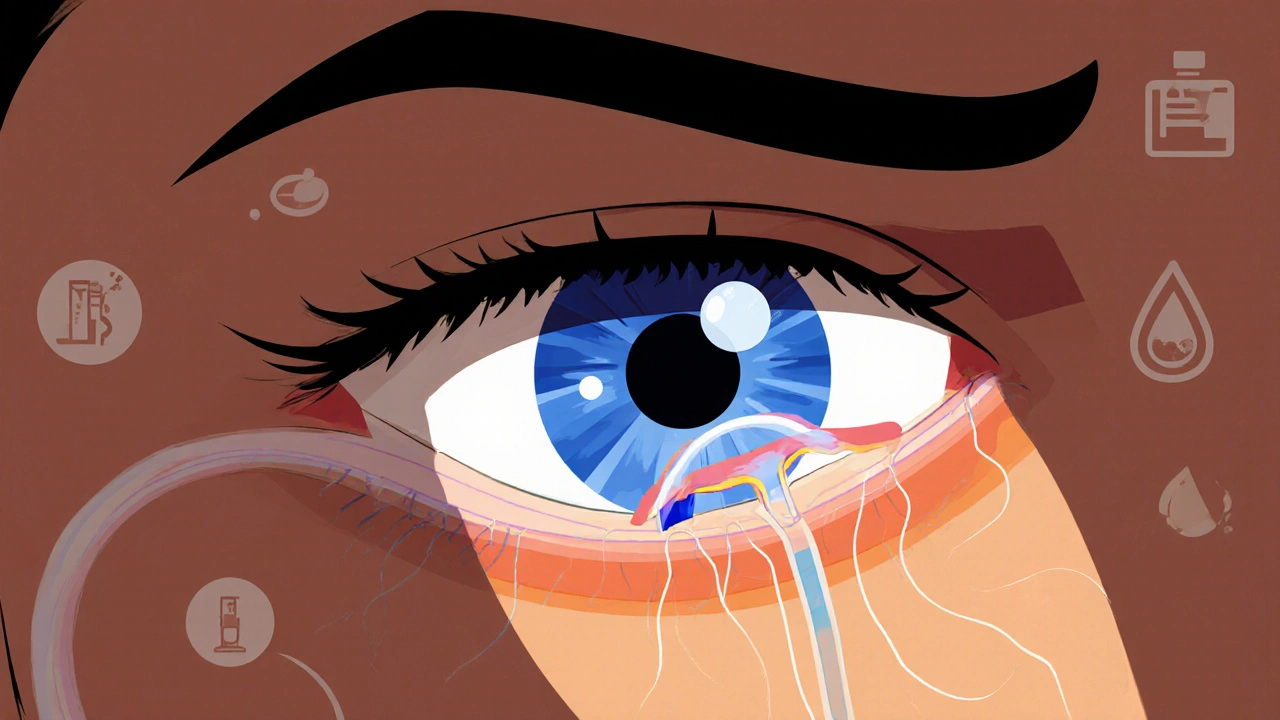
Trabeculectomy isn’t new - it was developed in the 1960s and still holds the title of most effective surgery for lowering eye pressure. The goal is simple: create a new drainage channel so fluid can leave the eye more easily. Surgeons make a small flap in the white part of the eye (sclera), remove a tiny piece of the drainage tissue (trabecular meshwork), and let fluid slowly leak out under the conjunctiva. This forms a small blister-like pocket called a bleb, which acts like a natural pressure valve. This procedure cuts IOP by 40-60% in most patients, often bringing pressure down to 5-15 mmHg. That’s critical for people with advanced glaucoma, where targets are below 15 mmHg. It’s also the go-to option for younger patients who need long-term control - because while it’s more intense upfront, it lasts. But it’s not simple. The surgery takes about an hour. Recovery isn’t quick: you’ll need 4-6 weeks of careful monitoring. Blebs can leak, get infected, or scar over. About 10-15% of patients deal with bleb leaks, and 10-20% see the bleb fail within five years. Serious complications like endophthalmitis (a rare but dangerous eye infection) happen in 0.5-2% of cases. That’s why follow-up visits are intense - doctors may need to adjust sutures, do needling to break up scar tissue, or even inject anti-scarring drugs.What MIGS Is and Why It’s Changing Glaucoma Care
MIGS stands for minimally invasive glaucoma surgery. These procedures, introduced around 2012, are designed to be safer, faster, and less disruptive. They use tiny incisions - often less than 1.5mm - and work with the eye’s natural drainage system instead of creating new ones. Most MIGS devices are implanted during cataract surgery, which makes them convenient for older patients who need both procedures. Popular MIGS options include:- iStent inject: Two microscopic stents placed in the drainage angle. Reduces pressure by 20-30% and cuts medication use by 1.5-2 drops on average.
- Hydrus Microstent: A tiny 8mm scaffold that opens the drainage channel. Works well with cataract surgery.
- Xen Gel Stent: A soft, 6mm tube that shunts fluid to the space under the conjunctiva. It’s more invasive than other MIGS but still safer than trabeculectomy.
- GATT (gonioscopy-assisted transluminal trabeculotomy): A suture is threaded through the drainage system to open it up. Achieves 30-35% IOP reduction.
How They Compare: Pressure, Safety, and Recovery
Here’s how trabeculectomy and MIGS stack up in real-world terms:| Feature | Trabeculectomy | MIGS |
|---|---|---|
| Average IOP Reduction | 40-60% | 20-30% |
| Typical Final IOP | 5-15 mmHg | 15-18 mmHg |
| Surgery Time | 60 minutes | 10-20 minutes |
| Recovery Time | 4-6 weeks | 1-2 weeks |
| Complication Risk | 5-15% | 1-3% |
| Post-op Monitoring | 3-6 months | 1-2 months |
| Cost (per eye, 2025) | $4,200 | $5,500-$6,300 |
| Best For | Advanced glaucoma, young patients, low target IOP | Mild-to-moderate glaucoma, patients wanting faster recovery |
One key point: MIGS doesn’t replace trabeculectomy - it changes who gets it. If you’re 70, have mild glaucoma, and are getting cataract surgery, MIGS is often the smartest choice. If you’re 40 with advanced disease and need pressure below 12 mmHg, trabeculectomy is still the most reliable option.

The Role of Laser: Why SLT Comes First
Before you even consider surgery, you’ll likely be offered Selective Laser Trabeculoplasty (SLT). It’s not surgery - it’s a quick, in-office laser treatment that takes 5-10 minutes. SLT uses low-energy pulses to stimulate the drainage system without damaging tissue. It’s safe, repeatable, and now the first-line treatment for open-angle glaucoma. The 2023 LiGHT trial changed everything. It showed SLT was just as good as daily eye drops at controlling pressure over three years - 75.3% of SLT patients stayed at target IOP versus 73.2% on drops. And 95% of SLT patients kept their quality of life, compared to 89% on medication. Because of this, major guidelines now say: start with SLT, not drops. Even newer versions like Direct Selective Laser Trabeculoplasty (DSLT) treat the whole drainage angle automatically, without touching the eye. It’s a bit more irritating afterward, but it’s faster and just as effective. For many, SLT delays or even avoids surgery entirely.What’s Next? The Future of Glaucoma Surgery
The field is moving fast. MIGS adoption is growing - it now makes up 65% of standalone glaucoma surgeries in the U.S. That’s because patients want less downtime and fewer risks. But long-term data (beyond 5 years) is still limited for many MIGS devices. Newer approaches are emerging too. Suprachoroidal shunts - tiny devices placed between layers of the eye wall - are showing promise as standalone treatments. They bypass the traditional drainage system entirely and may become options for patients who’ve failed other surgeries. The trend? Earlier intervention. Instead of waiting until medications fail, doctors are now using SLT and MIGS sooner. The goal isn’t just to delay surgery - it’s to prevent progression before vision loss happens.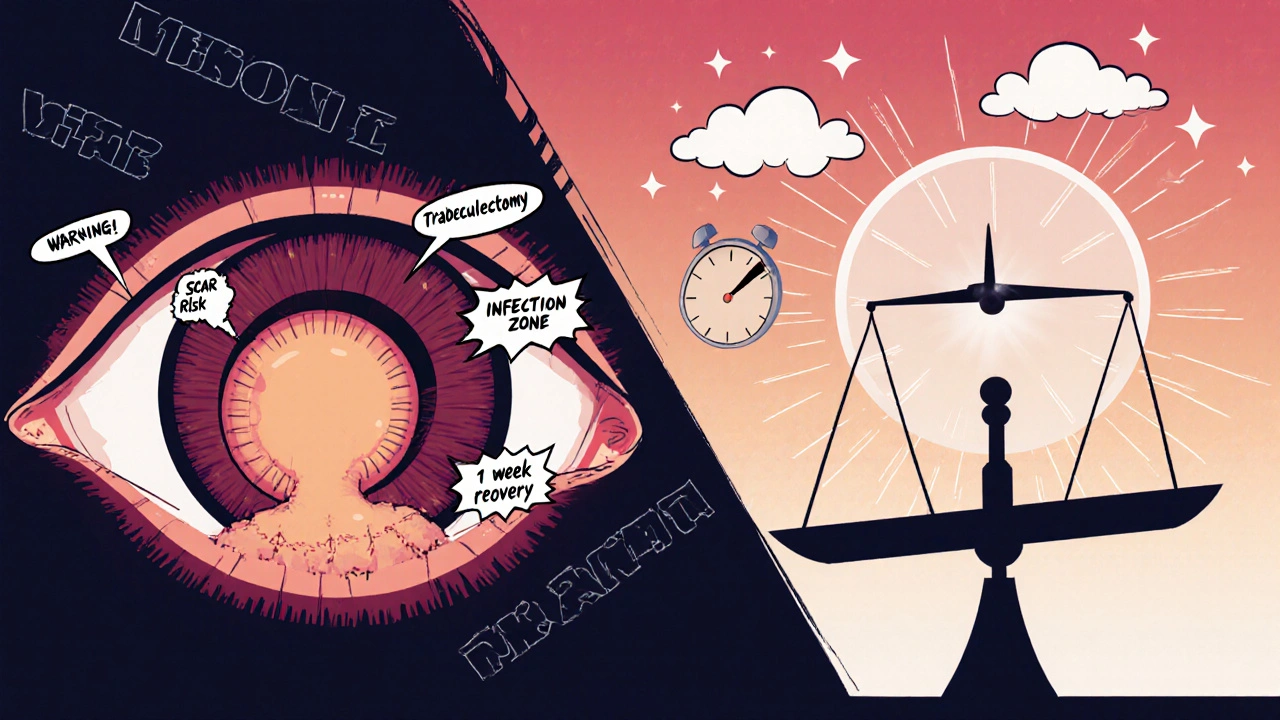
What Should You Do?
Your best move? Talk to your eye doctor about three things:- What’s your current IOP and how far has your vision already been affected?
- Are you already on eye drops? How many? Are they causing side effects?
- Do you have cataracts? If yes, combining MIGS with cataract surgery might be your best path.
Is MIGS better than trabeculectomy?
It depends. MIGS is safer, faster, and better for mild-to-moderate glaucoma. Trabeculectomy lowers pressure more and lasts longer - making it better for advanced cases or younger patients who need very low eye pressure. MIGS doesn’t replace trabeculectomy; it changes who needs it.
Can you have MIGS without cataract surgery?
Yes. While many MIGS procedures are done during cataract surgery, they can also be performed alone. Standalone MIGS is common for patients with mild-to-moderate glaucoma who don’t need cataract removal yet. Recovery is still quick - usually 1-2 weeks.
How long does a trabeculectomy last?
The pressure-lowering effect usually lasts for years, but the bleb can scar over or leak. About 80-90% of patients have good pressure control at one year. By five years, 10-20% need additional procedures to fix the bleb. Long-term success depends on careful follow-up and avoiding activities that strain the eye.
What’s the success rate of SLT?
In the LiGHT trial, 75.3% of patients maintained target eye pressure for three years after SLT - matching the results of daily eye drops. Success is higher in patients with higher baseline pressure and lower in those with advanced damage. SLT can be repeated if pressure rises again.
Is glaucoma surgery covered by insurance?
Yes. Medicare and most private insurers cover trabeculectomy, MIGS, and SLT when medically necessary. Out-of-pocket costs vary by region and facility, but the procedure itself is rarely denied if your doctor recommends it. Always check with your provider about specific device costs - some newer MIGS implants may have higher fees.
What to Watch For After Surgery
After any glaucoma surgery, keep an eye out for:- Sudden vision loss or increased pain - call your doctor immediately.
- Redness that gets worse instead of better.
- Flashes of light or floaters that appear suddenly.
- Fluid leaking from the eye (especially after trabeculectomy).


Anne Nylander
Just had MIGS with my cataract surgery last month and WOW. No more drops, no more burning eyes, and I can actually see my grandkids’ faces without squinting. Recovery was a breeze - back to gardening in 10 days. If you’re on the fence, DO IT. Your future self will thank you. 🌸