By January 2026, there are still 270 active drug shortages in the U.S.-and nearly all of them are generic medications. These aren’t rare or obscure drugs. They’re the ones millions of people rely on every day: antibiotics, heart medications, chemotherapy agents, and even basic IV fluids. When these drugs disappear from shelves, it’s not just an inconvenience-it’s a direct threat to patient safety.
Why Generic Drugs Are Most at Risk
Generic drugs make up 90% of all prescriptions filled in the U.S., but they account for over 70% of all shortages. Why? Because the business model doesn’t reward reliability. Manufacturers earn just 5-10% gross margins on many generic injectables, compared to 30-40% for brand-name drugs. When profits are this thin, companies cut corners. They delay maintenance on aging equipment. They skip investments in backup systems. And if one factory shuts down for a quality issue, there’s often no one else who can make the drug.Take sterile injectables-like vancomycin, cisplatin, or sodium bicarbonate. These account for about 60% of all shortages. Why? Because making them requires clean rooms, sterile processes, and precise temperature controls. One tiny contamination can shut down an entire production line. And there are rarely more than one or two FDA-approved manufacturers for each of these drugs. When one fails, the entire country feels it.
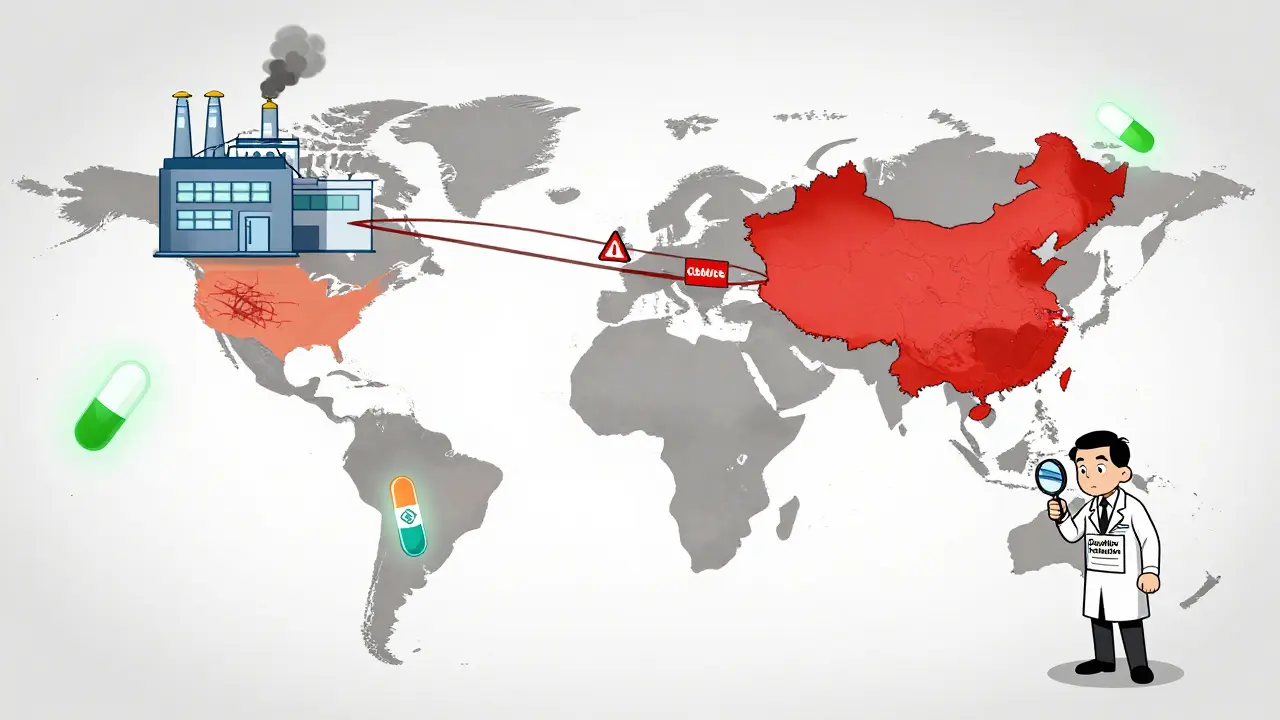
The Global Supply Chain Is a Single Point of Failure
More than half of all drugs used in the U.S. are made overseas. Eighty percent of the active ingredients come from just two countries: China and India. These facilities are often far from U.S. regulators. Inspections are infrequent. Quality controls vary. In 2024, FDA inspection citations for manufacturing violations jumped 35% from 2020 levels. One factory in India can hold up a drug for millions of Americans-because no one else is licensed to make it.This isn’t a new problem. It’s been building for years. Since 2015, the number of U.S.-based generic drug manufacturing facilities has dropped by 22%. Meanwhile, the top 10 generic drugmakers now control 60% of the market-up from 45% a decade ago. Consolidation sounds efficient, but it’s made the system more fragile. Fewer players means fewer backups. Fewer backups mean more shortages.
What Happens When a Drug Disappears?
When a generic drug runs out, it doesn’t just vanish. It triggers a chain reaction.- Hospitals delay cancer treatments because cisplatin isn’t available.
- Emergency rooms see more patients in pain because opioid generics are out of stock.
- Pharmacists spend 12-20 hours a week tracking down alternatives, updating systems, and calling other pharmacies.
- Patients abandon prescriptions because the substitute costs three times as much.
A 2024 survey found that 89% of U.S. hospitals have had to postpone treatments due to drug shortages. Oncology units were hit hardest: 67% reported changing chemotherapy protocols. That’s not theoretical. It’s real people getting less effective, riskier treatments because the original drug isn’t there.
And it’s not just hospitals. Independent pharmacies report that 43% of patients walk away from prescriptions during shortages-not because they don’t need the drug, but because the alternative is too expensive or hard to get.
Price Doesn’t Drop When Supply Does
One of the biggest myths about generics is that they’re cheap because competition keeps prices low. But when a drug goes short, that competition disappears. And prices spike.Generic drugs in shortage see a median price increase of 14.6%. But the real shock comes from substitutes. If you can’t get the original drug, you’re forced to use a different one-and those prices often jump three times faster than the original. A drug that cost $10 might now cost $30, $40, or even $50. For patients on fixed incomes, that’s not a choice. It’s a denial of care.
Brand-name drugs don’t behave the same way. Even when they’re in short supply, their prices usually stay flat. Why? Because they have patent protection, brand loyalty, and pricing power. Generics don’t. And that’s exactly why they’re the ones disappearing.
Healthcare Workers Are Burning Out
Managing drug shortages isn’t a side task. It’s a full-time job. Pharmacists now spend 15-20 hours a week just tracking shortages-finding alternatives, updating electronic records, training staff, and documenting every substitution. That’s time taken away from patient counseling, medication reviews, or even lunch breaks.And it’s happening while pharmacies are already understaffed. Seventy-two percent of hospitals say drug shortages have made their staffing crisis worse. Pharmacists aren’t trained to be supply chain detectives. They’re trained to ensure safe, effective care. Now they’re forced to juggle logistics, pricing, and risk-while knowing one wrong substitution could hurt a patient.

Policy Changes Have Helped-But Not Enough
There have been attempts to fix this. In 2020, the U.S. government launched the Essential Medicines List under Executive Order 14050. It helped. Shortages of those critical drugs dropped by 32% between 2020 and 2023.But the gains didn’t last. By 2023, shortages began climbing again. The FDA’s 2024 Drug Shortage Task Force laid out four clear solutions: diversify manufacturing locations, reward reliable suppliers, adopt advanced manufacturing tech, and build early warning systems. All sound good. None have been fully implemented.
Worse, new threats are emerging. Proposed tariffs of 50-200% on imported pharmaceuticals could disrupt the already fragile supply chain. Analysts warn it could spike shortages of chemotherapy drugs and IV fluids even further. The Congressional Budget Office now predicts over 350 active shortages by the end of 2026-if nothing changes.
What Needs to Change
The system isn’t broken because of bad actors. It’s broken because the rules reward the lowest price over the safest supply. Until manufacturers are paid enough to invest in quality, redundancy, and reliability, shortages will keep happening.What could help?
- Guaranteed minimum prices for essential generics-enough to cover production, quality control, and backup capacity.
- Financial incentives for manufacturers who maintain multiple production sites.
- Fast-tracking approvals for new suppliers of critical drugs.
- Public reporting of real-time inventory levels for high-risk drugs.
Right now, the market doesn’t care if a drug is available. It only cares if it’s cheap. That’s not a market failure. It’s a policy failure. And patients are paying the price-with their health, their time, and sometimes their lives.
Why This Matters Everywhere
You might think this is just a U.S. problem. It’s not. The same manufacturing hubs supply drugs to Canada, Australia, and Europe. When a factory in India shuts down, it doesn’t just affect American hospitals. It affects clinics in Melbourne, Toronto, and London too. Global supply chains don’t recognize borders.And as aging populations demand more medications-and as more drugs go generic-the pressure will only grow. Without real reform, we’re not just facing shortages. We’re facing a system that’s designed to fail.
Why are generic drug shortages so common compared to brand-name drugs?
Generic drugs are more commonly in shortage because they’re sold at very low prices, leaving manufacturers with razor-thin profit margins-often just 5-10%. This makes it hard to invest in quality equipment, backup production lines, or regulatory compliance. Brand-name drugs, by contrast, have patent protection and higher margins, so companies can afford to maintain multiple manufacturing sites and keep safety buffers. Even when brand-name drugs are in short supply, alternatives are often available. For generics, they rarely are.
Which types of generic drugs are most likely to be in short supply?
Sterile injectables are the most vulnerable. This includes antibiotics like vancomycin, chemotherapy drugs like cisplatin, IV fluids like saline, and critical cardiac medications. These require complex, sterile manufacturing environments that only a few facilities can handle. They also have the lowest profit margins, so manufacturers are less likely to invest in redundancy. About 60% of all drug shortages involve sterile injectables.
How do drug shortages affect patient outcomes?
A 2022 AMA survey found that 63% of pharmacists reported drug shortages led to serious patient harm. This includes delayed cancer treatments, increased infection risks from substituted antibiotics, uncontrolled pain due to opioid shortages, and even deaths when life-saving drugs aren’t available. Patients often get less effective, more expensive, or riskier alternatives. In some cases, they simply don’t get treated at all.
Why can’t we just make more generic drugs in the U.S.?
The number of U.S.-based generic manufacturing facilities has dropped 22% since 2015, from 1,842 to 1,437. Building new facilities is expensive, and without guaranteed pricing or long-term contracts, companies won’t invest. The global market is flooded with low-cost imports, so U.S. manufacturers can’t compete on price alone. Without policy changes that reward reliability over cheapness, there’s no financial reason to build more here.
Do tariffs on imported drugs make shortages worse?
Yes. Over 80% of active pharmaceutical ingredients come from China and India. Tariffs of 50-200% on these imports would raise production costs, reduce profit margins further, and likely cause manufacturers to cut back or stop production altogether. Analysts warn this could trigger shortages of chemotherapy drugs, IV fluids, and other essentials. It’s like putting a tax on life-saving medicine.
Is there any progress being made to fix this?
There have been small wins. The Essential Medicines List created in 2020 cut shortages of critical drugs by 32% for a few years. The FDA now tracks shortages more closely and encourages early reporting. But these are temporary fixes. The core issue-low prices that disincentivize quality and reliability-hasn’t been addressed. Without changing how generics are priced and reimbursed, shortages will keep coming back.



blackbelt security
My cousin’s a pharmacist in Ohio. She told me last week she spent 18 hours just trying to find a replacement for vancomycin. No one had it. Not one pharmacy. She had to call 14 different suppliers. Patients were crying in the parking lot. This isn’t a policy issue-it’s a moral emergency.
Someone needs to pay manufacturers to keep backup lines running. Not ‘maybe someday.’ Now.
And stop pretending ‘free markets’ fix this. They don’t. They just make it worse.