Drug-Induced Pulmonary Fibrosis Risk Checker
Check Your Medication Risk
Your Risk Assessment
Medications Selected:
Common Early Symptoms:
- Dry, persistent cough (not from allergies or cold)
- Shortness of breath during light activity
- Unexplained fatigue or joint pain
- Fever or chills without infection
Most people assume that if a drug is approved and prescribed, it’s safe. But some medications quietly scar your lungs over time - no warning, no obvious signs until it’s too late. This isn’t rare. It’s called drug-induced pulmonary fibrosis, and it’s one of the most dangerous side effects doctors don’t always talk about.
What Exactly Is Drug-Induced Pulmonary Fibrosis?
Drug-induced pulmonary fibrosis (DIPF) happens when certain medications trigger inflammation and permanent scarring in the tiny air sacs of your lungs. These sacs, called alveoli, are where oxygen enters your blood. When scar tissue builds up, they stiffen and can’t expand properly. Breathing becomes harder - not just when you run, but even when you sit still or get dressed.
Unlike lung damage from smoking or pollution, DIPF isn’t caused by long-term exposure to toxins. It’s an unpredictable reaction. One person takes the same drug for years with no issues. Another develops severe scarring in months. The reason? No one knows for sure. Genetics, age, and unknown biological factors play a role - but there’s no test to predict who’s at risk.
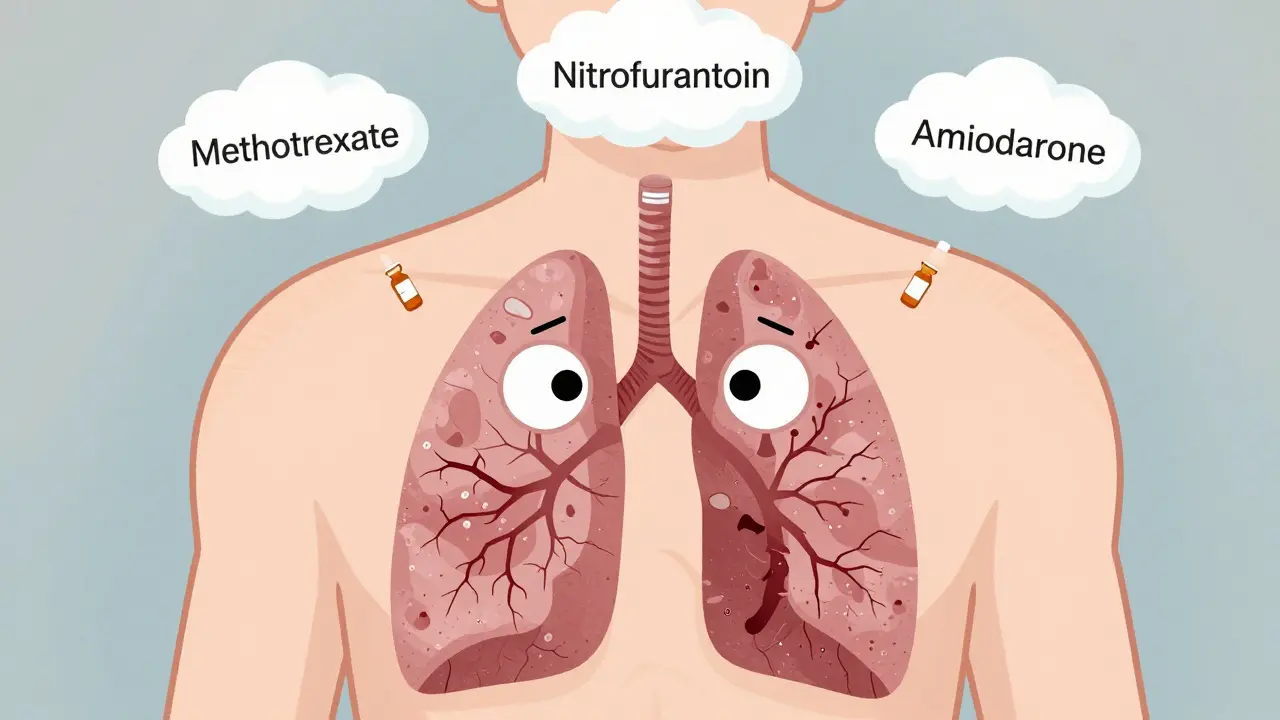
The Top Medications That Can Scar Your Lungs
Over 50 medications have been linked to pulmonary fibrosis. But three stand out as the most common culprits - and they’re prescribed to millions every year.
- Nitrofurantoin: Used for urinary tract infections, especially in older women. It’s often taken for months as a preventive. But after 6 months to 10 years, some patients start coughing and gasping. In New Zealand, it was the #1 reported drug linked to lung scarring between 2014 and 2024 - with 47 confirmed cases.
- Methotrexate: A common treatment for rheumatoid arthritis and psoriasis. About 3-7% of users develop lung inflammation that can turn into fibrosis. It often hits fast - sudden cough, fever, and breathlessness. Many patients are told they have a cold or flu. By the time it’s caught, damage is already done.
- Amiodarone: Prescribed for irregular heart rhythms. It’s effective, but toxic to lungs over time. After taking more than 400 grams total (usually 6-12 months of daily use), up to 7% of patients develop scarring. The worst part? Symptoms can appear even after stopping the drug.
Chemotherapy drugs like bleomycin and cyclophosphamide are also high-risk. Bleomycin causes lung damage in up to 20% of patients. These drugs are used in cancer treatment, so doctors expect some side effects - but many don’t realize the lung damage can be permanent even after stopping treatment.
Newer cancer drugs called immune checkpoint inhibitors (like pembrolizumab and nivolumab) are now showing up in reports. These drugs boost the immune system to fight tumors - but sometimes they turn it against the lungs. Cases are still rare, but rising fast.
How Do You Know If It’s Your Medication?
Early symptoms are easy to ignore:
- A dry, persistent cough - not from allergies or a cold
- Shortness of breath during light activity - climbing stairs, walking to the mailbox
- Unexplained fatigue or joint pain
- Fever or chills without infection
These symptoms don’t show up right away. For nitrofurantoin, it can take years. For methotrexate, it might be weeks. Many patients are told they’re just getting older. One Reddit user from Melbourne wrote: “I thought my breathlessness was just from being 72. Turns out it was methotrexate. I had 15% lung function left by the time they figured it out.”
Diagnosis is tricky. There’s no single test for DIPF. Doctors must rule out other causes - infections, autoimmune diseases, environmental exposure. A high-resolution CT scan often shows the telltale honeycomb pattern of scar tissue. But without knowing your full medication history, even the best scan can miss it.

What Happens After Diagnosis?
There’s no cure for scarred lung tissue. But stopping the drug early can stop the damage - and sometimes reverse it.
The first step? Stop taking the medication - immediately. Under doctor supervision. Never quit cold turkey, especially with heart or cancer drugs.
Most patients (89%) start improving within 3 months after stopping the drug. But recovery isn’t guaranteed. About 15-25% end up with permanent lung damage. If the scarring is advanced, oxygen therapy or even a lung transplant may be needed.
Corticosteroids like prednisone are often used to calm inflammation. Doses start high - 0.5 to 1 mg per kg of body weight - then slowly taper over 3 to 6 months. Oxygen is added if blood oxygen levels drop below 88%.
Follow-up is critical. Pulmonary function tests every 3-6 months track whether your lungs are healing or worsening. If you’re on any of these drugs, ask your doctor for a baseline lung test before you start - and another after 6 months.
Why Isn’t This More Widely Known?
A 2022 survey found only 58% of primary care doctors routinely ask patients on high-risk drugs about breathing problems. Many don’t realize these side effects exist. Pharmacists don’t always warn patients. Drug labels mention “lung toxicity” in tiny print - if at all.
New Zealand’s health agency, Medsafe, issued a public alert in December 2024 after reviewing 173 cases of drug-induced lung scarring between 2014 and 2024. Thirty people died. The report said: “Patients must be informed of this risk before starting treatment.” But in practice, that rarely happens.
The number of reported cases has jumped 23.7% over the past decade. That’s not just better reporting - it’s more people getting sick. As new drugs flood the market, especially targeted cancer therapies and biologics, the list of dangerous medications keeps growing.

What You Can Do
If you’re taking any of these drugs, here’s what to do now:
- Know your meds. Make a list of every prescription, even over-the-counter ones. Check if any are linked to lung damage.
- Watch your breathing. If you develop a new cough or shortness of breath - even mild - don’t wait. Tell your doctor immediately. Say: “Could this be drug-induced lung damage?”
- Ask for a baseline test. Request a spirometry or DLCO test before starting high-risk drugs. It’s quick, painless, and gives you a reference point.
- Don’t ignore symptoms. If you’ve been on nitrofurantoin for years, or methotrexate for arthritis, and you’re suddenly winded - get checked. Delayed diagnosis means irreversible damage.
There’s no magic pill to prevent this. But awareness saves lives. If you’re on one of these drugs, you’re not being paranoid - you’re being smart.
What’s Next?
Researchers are working on blood tests that could predict who’s at risk before damage starts. Early trials are looking at genetic markers and immune proteins that might signal trouble. But those tests aren’t available yet.
In the meantime, the best defense is knowledge. Talk to your doctor. Ask questions. Push for answers. And if you’ve been told your breathlessness is just aging - get a second opinion.
Scarring in the lungs doesn’t heal. But catching it early? That’s your best shot at keeping your lungs working - and your life moving.
Can drug-induced pulmonary fibrosis be reversed?
Yes - if caught early. Stopping the offending drug immediately can stop further scarring and allow some healing. About 89% of patients see improvement within 3 months. But if the fibrosis is advanced, the damage is permanent. Recovery depends on how soon the drug is stopped and how much scar tissue has formed.
Which drugs are most likely to cause lung scarring?
The top three are nitrofurantoin (for UTIs), methotrexate (for arthritis), and amiodarone (for heart rhythm). Chemotherapy drugs like bleomycin and cyclophosphamide are also high-risk. Newer cancer immunotherapies like pembrolizumab are increasingly linked to lung damage. These are not rare side effects - they’re well-documented.
How long does it take for lung damage to develop?
It varies. Nitrofurantoin can take 6 months to 10 years. Methotrexate often causes symptoms within weeks to months. Amiodarone usually appears after 6-12 months of use. Bleomycin can cause damage after just a few doses. There’s no safe timeline - it depends on your body, not the dose.
Are there tests to detect drug-induced lung damage early?
Yes - but they’re not always done. A high-resolution CT scan shows scarring clearly. Pulmonary function tests (spirometry and DLCO) measure how well your lungs move air and transfer oxygen. These should be done before starting high-risk drugs and repeated every 6 months. Blood tests for early detection are still in research.
Should I stop taking my medication if I have a cough?
Don’t stop on your own. Call your doctor immediately. Some drugs, like amiodarone or methotrexate, can’t be stopped abruptly. Your doctor will assess your symptoms, order tests, and guide you on safely discontinuing the drug if needed. The goal is to stop the drug before the damage becomes permanent.
Is drug-induced pulmonary fibrosis common?
It’s not rare. About 5-10% of all interstitial lung disease cases are drug-induced. In New Zealand alone, 173 cases were reported between 2014 and 2024 - with 30 deaths. The number of cases is rising, partly because more drugs are being used and partly because doctors are starting to recognize it. But many cases are still missed.


Allie Lehto
I can't believe we're still letting Big Pharma get away with this. 😔 My aunt took nitrofurantoin for a UTI and ended up on oxygen. They told her it was just "aging." No warning. No nothing. This is criminal.