Imagine waking up with joints so swollen you can’t grip a coffee cup. Or gasping for air during an asthma attack that won’t quit. For many people, corticosteroids are the difference between being stuck in bed and getting through the day. They work fast-sometimes in under 48 hours. But here’s the catch: what helps today might hurt you tomorrow.
How Corticosteroids Work (And Why They’re So Fast)
Corticosteroids are synthetic versions of cortisol, the stress hormone your body naturally makes. When you’re inflamed-whether from arthritis, asthma, or an autoimmune flare-your immune system goes into overdrive. Corticosteroids don’t just calm it down; they shut it off. That’s why they’re the go-to for acute flare-ups.
Unlike disease-modifying drugs that take weeks to kick in, corticosteroids like prednisone or methylprednisolone start working in hours. A 2021 study in Arthritis & Rheumatology showed they cut joint pain and swelling twice as fast as NSAIDs. For someone with lupus or rheumatoid arthritis, that speed can mean avoiding the hospital. In severe asthma, a short course can reduce hospital stays by nearly two days.
They come in many forms: pills, injections into joints or muscles, inhalers, creams, and IV drips. Oral pills are the most common-68% of all prescriptions, according to the American Academy of Family Physicians. Injections? They’re popular for knee or shoulder pain. Relief can take up to seven days to peak, but once it hits, it lasts weeks to months.
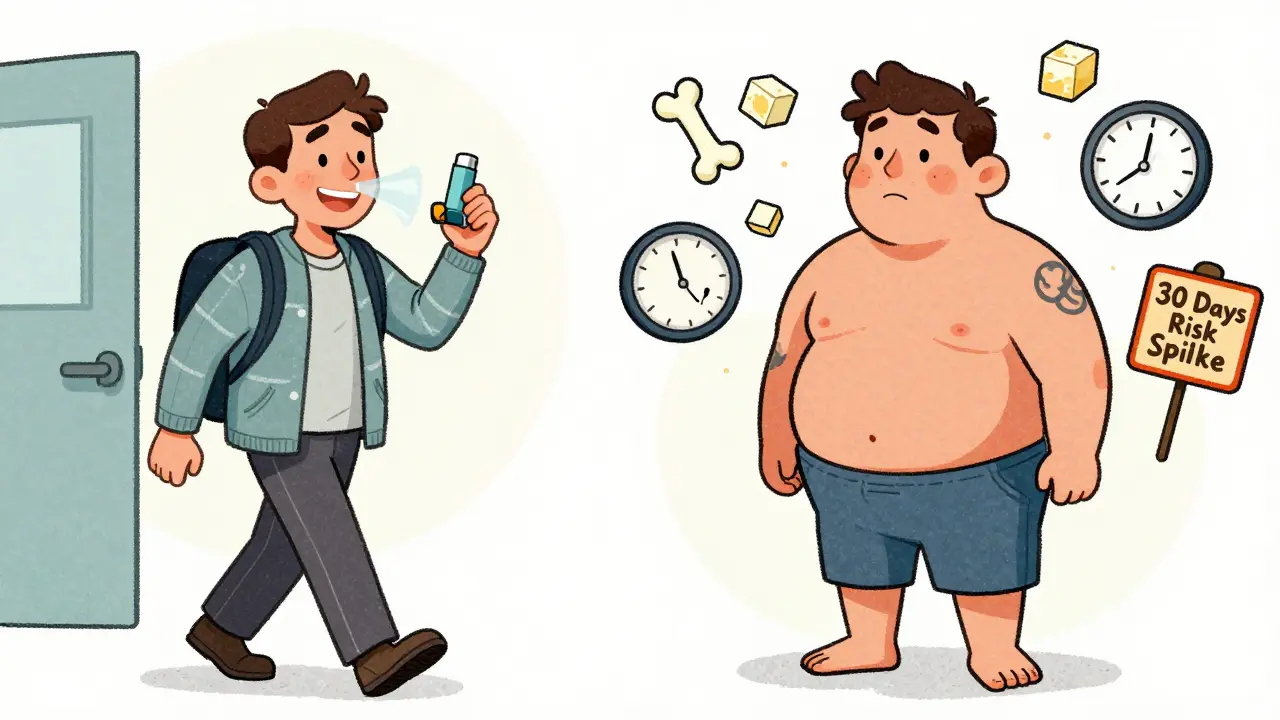
The Hidden Cost: What Happens After the Relief
That rapid relief doesn’t come free. The same 2021 study that praised corticosteroids’ speed also found they spike serious risks within just 30 days:
- 430% higher chance of sepsis
- 230% higher risk of blood clots
- 90% higher risk of fractures
And those are just the big ones. Most people notice the smaller, but still troubling, changes first:
- Weight gain-especially around the face and belly (moon face, buffalo hump)
- Insomnia, mood swings, or anxiety
- High blood sugar-even in people without diabetes
- Thinning skin that bruises easily
A 2023 survey of 1,200 corticosteroid users found 87% gained weight (average 12.4 pounds in 8 weeks), 63% had trouble sleeping, and 41% needed new diabetes meds. One Reddit user wrote: “I started 10mg of prednisone for a rash. Two weeks later, I looked like a different person-and my blood sugar was through the roof.”
Long-Term Use: The Point of No Return
Doctors agree: corticosteroids should never be a long-term solution. But many people end up on them anyway.
The American College of Rheumatology says no one should stay on systemic corticosteroids longer than 12 weeks unless absolutely necessary. Yet, 29% of long-term users (over 3 months) report permanent damage-even after stopping:
- 12% developed cataracts
- 8% got osteoporosis
- 7% were diagnosed with steroid-induced diabetes
Bone loss starts within the first month. You can lose 3-5% of bone density each month on high doses. That’s why experts now recommend DEXA scans for anyone on more than 7.5mg of prednisone daily for over three months. Calcium and vitamin D aren’t optional-they’re lifesavers. Some patients even need annual IV bone meds like zoledronic acid.
And here’s the scary part: a 2023 meta-analysis found every extra month of corticosteroid use beyond three months raises your 10-year death risk by 4.7%. That’s not a small number. It’s why the European League Against Rheumatism now says: “No patient should be on daily steroids longer than six months without proving they’ve tried at least two stronger, targeted therapies.”
When Are Corticosteroids Actually Needed?
Not every sniffle or backache needs steroids. Yet, nearly half of all prescriptions are for conditions where they offer little to no benefit.
According to IQVIA data analyzed by the AAFP:
- 22% of prescriptions were for acute bronchitis
- 19% were for nonspecific back pain
- Only 18% were for true autoimmune conditions like lupus or vasculitis
Dr. Robert Simon from NYU put it bluntly: “Giving steroids for a cold or a sore throat isn’t just ineffective-it’s dangerous.”
Real evidence-backed uses are limited to:
- Severe asthma or COPD flare-ups (5-day max courses)
- Flares of rheumatoid arthritis, lupus, or multiple sclerosis
- Severe allergic reactions or anaphylaxis
- Peritonsillar abscess (reduces need for surgery by 27%)
For most other conditions-sinus infections, earaches, minor allergies-there are safer options. Antibiotics, antihistamines, or even just time do the job without the risk.
How to Use Them Safely (If You Must)
If your doctor prescribes corticosteroids, here’s what you need to do:
- Ask for the shortest course possible. Three days? Five? Ten? Push back if they say “two weeks.”
- Never stop cold turkey. Your body shuts down natural cortisol production. Stopping suddenly can cause adrenal crisis-low blood pressure, vomiting, even death. Tapering over at least 7 days is non-negotiable.
- Monitor your blood sugar. Even if you’ve never had diabetes, check it weekly if you’re on more than 10mg daily.
- Protect your bones. Take 1,200mg calcium and 800 IU vitamin D daily. Ask about a DEXA scan if you’re on it longer than 3 months.
- Watch for infection signs. Fever, chills, or a sore throat that won’t go away? Call your doctor immediately. Your immune system is suppressed.
Also, tell every doctor you see-even your dentist-that you’ve taken steroids in the last year. If you need surgery or a major procedure, you may need a stress dose of hydrocortisone to keep your body from crashing.

What’s Changing in 2026?
There’s new hope on the horizon. In December 2023, the FDA approved the first selective glucocorticoid receptor modulator-fosdagrocorat. It works like a steroid but with far fewer side effects. In trials, it caused 63% less high blood sugar than prednisone at the same anti-inflammatory dose.
Hospitals are also getting smarter. In 87% of U.S. hospitals, EHR systems now flag inappropriate steroid prescriptions. Medicare Advantage plans now require pre-authorization for any course longer than 10 days. These changes have already cut unnecessary prescriptions by 31% in early adopter systems.
But the biggest shift is cultural. Doctors are finally treating corticosteroids like a controlled substance-not a quick fix. The message is clear: use them hard, use them fast, use them briefly. And never, ever use them as maintenance.
What Patients Are Saying
On Healthgrades, corticosteroids have a 3.2 out of 5 rating. Why? Because 68% say they saved their life during a flare. But 79% say they paid a heavy price.
One user wrote: “Prednisone got me out of the ER. But it took me two years to lose the weight, and I still have cataracts.”
Another: “I thought the moon face would go away. It didn’t. My skin’s still thin. My bones are fragile. I’m 35. I shouldn’t be this broken.”
These aren’t rare stories. They’re the cost of fast relief.
Are corticosteroids safe for short-term use?
Short-term use (under 14 days) is generally safe for most people when used correctly. But even brief courses can raise risks of infection, blood clots, and high blood sugar. The key is using them only when necessary and under medical supervision. Never take them for viral infections like colds or flu-they won’t help and could make things worse.
Can I stop taking corticosteroids if I feel better?
No. Stopping suddenly can trigger adrenal insufficiency-a life-threatening condition where your body can’t produce enough cortisol. Even if you feel fine, you must taper down slowly over days or weeks, depending on how long you’ve been on them. Your doctor should give you a clear tapering schedule. If they don’t, ask for one.
Do steroid injections cause less harm than pills?
Injections deliver the drug locally, so systemic side effects are lower-but not gone. One joint injection still sends some steroids into your bloodstream. Repeated injections can weaken tendons and cartilage over time. They’re great for flare-ups, but shouldn’t be used more than 3-4 times a year in the same joint. Always combine them with physical therapy, not as a replacement.
Is there a natural alternative to corticosteroids?
There’s no natural substitute that works as fast or as powerfully. Turmeric, omega-3s, and CBD may help with mild inflammation, but they won’t stop a severe autoimmune flare. For acute, life-altering inflammation, corticosteroids are still the gold standard. The goal isn’t to avoid them entirely-it’s to use them wisely and get off them as soon as possible.
How do I know if I’m on too high a dose?
Signs you’re on too much include rapid weight gain (especially face and belly), persistent high blood sugar, mood swings, trouble sleeping, or easy bruising. If you’ve been on more than 10mg of prednisone daily for over 3 weeks, your doctor should be monitoring your bone density, blood sugar, and eye health. If they’re not, ask why.
Final Thought: Use Them Like a Fire Extinguisher
Think of corticosteroids like a fire extinguisher. You don’t live with it on your kitchen wall 24/7-you grab it when the flames are roaring. Once the fire’s out, you don’t keep spraying. You put it back. You check the pressure. You make sure it’s ready for next time.
That’s how corticosteroids should be used. Fast. Focused. Brief. And never, ever left running.



Kunal Majumder
Man, I remember when I was on prednisone for that bad eczema flare. Felt like a superhero for a week - then like a balloon that got left in the sun. Weight gain, insomnia, weird mood swings… but honestly? Worth it to stop scratching my skin off. Just don’t let it become your new normal.