When your asthma flares up every spring, or after you vacuum, or even when your cat jumps on the bed - it’s not just bad luck. It’s likely allergic asthma. This isn’t just regular asthma with a sneeze attached. It’s your immune system mistaking harmless things like pollen, dust, or pet dander for invaders, and launching a full-scale attack inside your lungs. About 60% of adults and over 80% of kids with asthma in the U.S. have this form, according to the American College of Allergy, Asthma, and Immunology. That’s millions of people whose symptoms aren’t random - they’re tied to specific triggers you can actually identify and manage.
What Exactly Triggers Allergic Asthma?
Allergic asthma happens when your body overreacts to allergens through IgE antibodies. These antibodies flag things like pollen, mold, or cat dander as threats. When you breathe them in, your immune system releases chemicals that cause your airways to swell, tighten, and produce mucus. The result? Wheezing, coughing, chest tightness - the classic asthma symptoms, but with a clear cause.
Some triggers are seasonal. Tree pollen hits hardest in late winter and early spring - March in most temperate zones. Grass pollen peaks in June, and ragweed explodes in September. In Melbourne, where I live, spring means high levels of ryegrass pollen, which can spike above 100 grains per cubic meter on windy days. That’s enough to send even well-controlled asthmatics to the ER. Mold spores like Alternaria follow a different pattern - they surge after heavy rain or thunderstorms, especially in late summer. One study showed emergency visits for asthma jumped 3.5 times when Alternaria counts hit 500 spores per cubic meter.
Indoor triggers are even more constant. Dust mites thrive in warm, humid places - your mattress, pillows, carpets. The threshold for triggering symptoms? Just 2 micrograms of mite allergen per gram of dust. Guess what? Eighty-four percent of U.S. homes with humidity above 50% have that much. Cat allergen (Fel d 1) is even more sneaky. It’s sticky, lightweight, and clings to clothes and furniture. Even if you don’t own a cat, 79% of homes still have enough of it to cause problems. Dog allergen (Can f 1) is present in two-thirds of homes. And if you’ve ever walked into a friend’s house and suddenly started coughing - that’s why.
How to Avoid Allergens - For Real
Knowing your triggers is only half the battle. Avoiding them is the other half. And most people don’t do it right.
Start with your bedroom. Dust mites live in bedding. The most effective fix? Allergen-proof covers for your mattress, box spring, and pillows. Don’t just buy any zippered cover - look for ones certified to block particles under 10 microns. A queen set costs around $129, but it cuts your exposure by up to 90%. Wash your sheets weekly in hot water - at least 130°F. Cold water won’t kill the mites. Steam cleaning your mattress once a year helps too.
Next, your vacuum. Regular vacuums blow allergens back into the air. Use a HEPA-filter vacuum - and vacuum at least twice a week. One study showed this reduces cat allergen by 42%. I’ve seen people switch from a cheap model to a Dyson V15 and notice fewer nighttime coughs within weeks. Don’t forget to replace the filter every 6 months.
Control humidity. Keep indoor levels between 30% and 50%. Use a hygrometer to check - not a guess. Above 50%, dust mites multiply. Below 30%, your airways dry out and get irritated. A dehumidifier like the AprilAire 500M can drop humidity from 65% to 45% in a week, and dust mite levels drop from 20 µg/g to under 0.5 µg/g. That’s not a myth - it’s lab-tested.
For pollen, keep windows closed when counts exceed 9.7 grains per cubic meter - that’s the threshold the National Allergy Bureau uses to warn sensitive people. Check local pollen forecasts daily. Wear an N95 mask when mowing the lawn or raking leaves. It cuts exposure by 85%. And shower after being outside. Pollen sticks to your hair and clothes. If you don’t wash up, you’re bringing it into bed with you.
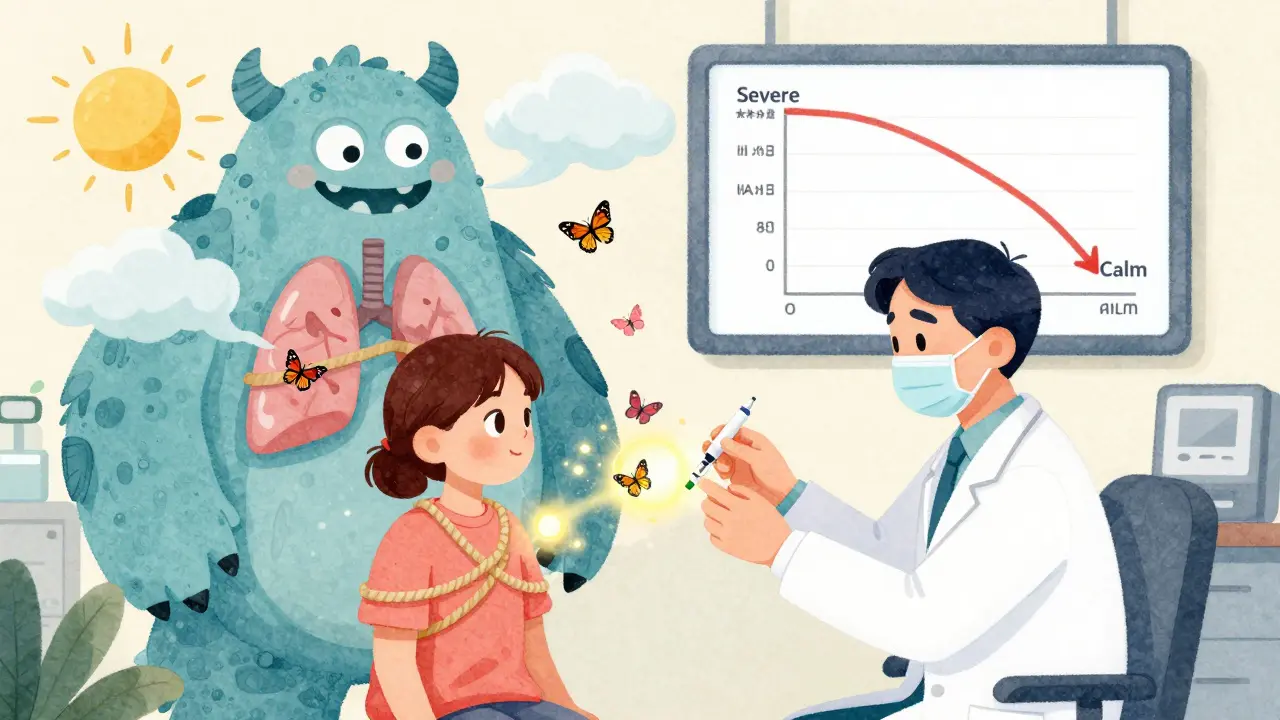
Immunotherapy: The Only Treatment That Changes the Disease
Medications like inhalers and antihistamines treat symptoms. But immunotherapy - allergy shots or drops - treats the cause. It’s the only asthma treatment that can actually change how your immune system responds to allergens.
There are two main types: subcutaneous immunotherapy (SCIT), or allergy shots, and sublingual immunotherapy (SLIT), which uses tablets or drops under the tongue. Both work by slowly exposing you to tiny, increasing doses of the allergen you’re sensitive to. Over time, your body learns not to overreact.
SCIT starts with weekly injections for 4 to 6 months, building up to a maintenance dose. Then you go every 2 to 4 weeks for 3 to 5 years. It’s effective - 70% to 80% of patients see big improvements after 12 to 18 months. A 2021 Cochrane review of over 12,000 people found immunotherapy reduced asthma symptoms by 30% to 50% more than medication alone. One patient in a study saw their IgE levels drop from 120 kU/L to 15 kU/L after three years of cat dander shots. Their asthma went from severe to nearly gone.
SLIT is easier - no needles. You take a tablet or drops daily. It’s great for people who hate shots. But it’s not perfect. About 78% of users get mild oral itching in the first month. That’s normal, but it’s why some quit. Still, for dust mite allergies, SLIT cuts symptom scores by 35% - better than inhaled steroids alone.
Costs vary. In the U.S., Medicare covers 80% of allergy shots. The copay is about $18.90 per injection. SLIT tablets like Grastek for grass allergy cost around $800 per year. But here’s the real math: if immunotherapy cuts your rescue inhaler use by 40%, and prevents one ER visit a year (which averages $3,000), you’re saving money in under two years.

Who Benefits Most - And Who Doesn’t
Not everyone with asthma has allergic asthma. And not everyone with allergies has asthma. That’s why testing matters. Skin prick tests or blood tests for specific IgE can confirm what you’re allergic to. A wheal larger than 3mm on a skin test means you’re sensitized. Blood IgE levels above 100 kU/L suggest allergic asthma. Above 400 kU/L? You’re likely in the severe category.
Immunotherapy works best for people with clear, measurable triggers - like house dust mites, pollen, or cat dander. It’s less effective if you’re allergic to multiple things, or if your asthma is mostly triggered by cold air, exercise, or pollution.
And here’s the catch: about 30% of people diagnosed with allergic asthma actually have non-type 2 inflammation. That means their immune system isn’t driven by IgE or eosinophils. Biologics and immunotherapy won’t help them - and they’ll waste thousands of dollars. That’s why doctors now check biomarkers like blood eosinophils (above 300 cells/µL) and FeNO (fractional exhaled nitric oxide above 25 ppb). If those are normal, your asthma might be something else.
That’s why diagnosis is key. Don’t assume your asthma is allergic just because you sneeze around cats. Get tested. If your symptoms improve when you avoid a specific trigger, that’s a clue. But only testing gives you certainty.
What’s New in 2025 - And What’s Coming
The field is moving fast. In 2024, the FDA approved CAT-PAD, a new peptide immunotherapy for cat allergy. Instead of 6 months of weekly shots, you get 8 weeks. It’s a game-changer for people who can’t stick with long-term treatment.
There’s also a new pollen vaccine in Phase III trials that needs only four doses a year. Early results show 60% fewer symptoms. And wearable tech is catching up. The Allergen Insight nasal sensor, now FDA-approved, detects allergens as low as 0.1 µg/m³ and sends alerts to your phone. If it picks up ragweed outside, you’ll know before you step out.
AI platforms like AsthmaIQ now combine pollen forecasts, your inhaler use, and even weather data to predict your next flare-up - with 92% accuracy. That’s not science fiction. It’s available now.
By 2030, doctors may use genetic tests to predict who will respond to immunotherapy. A marker called rs230548 on chromosome 17q21 already shows 85% accuracy in early studies. That means no more trial-and-error. You’ll know before you start whether it’ll work.
Real Stories, Real Results
One Reddit user in Melbourne shared their story: after replacing bedding, using a HEPA vacuum, and installing a dehumidifier, their peak flow jumped from 380 to 470 L/min over six months. They went from needing rescue inhalers twice a week to once a month.
Another case: a 12-year-old with severe cat allergy had wheals 15mm wide on skin tests. After three years of immunotherapy, they passed a challenge test - exposed to cat dander in a controlled setting - and had zero reaction. Their IgE dropped from 120 to 15 kU/L. They now pet cats without fear.
But it’s not magic. It takes time. It takes consistency. You can’t skip a week of SLIT because you’re busy. You can’t skip vacuuming because it’s raining. You can’t ignore humidity levels because it’s winter. Allergic asthma doesn’t care about your schedule. But if you stick with it, it gets better.
What to Do Next
If you suspect you have allergic asthma, start with this:
- Track your symptoms. When do they happen? After pets? After mowing? During spring? Write it down.
- Get tested. Ask your doctor for a skin prick test or IgE blood test. Know what you’re allergic to.
- Start with avoidance. Cover your mattress. Wash bedding weekly. Use a HEPA vacuum. Control humidity.
- If symptoms persist, talk to an allergist about immunotherapy. Don’t wait until you’re in the ER.
Allergic asthma isn’t a life sentence. It’s a condition with clear triggers - and real solutions. You don’t have to live with constant wheezing. You just need to know what’s causing it - and how to stop it.



jeremy carroll
bro i had no idea dust mites were that sneaky. switched to allergen-proof covers last spring and my nights actually feel like sleep now. no more 3am wheezing like a broken accordion. also started washing sheets in hot water - turns out cold water is just a fancy way of hosting a mite rave. 10/10 recommend.