Schizophrenia Symptom Explorer
Explore the three main categories of schizophrenia symptoms and learn how they impact daily life.
Positive Symptoms
Add experiences that aren't actually present, such as hallucinations and delusions.
Negative Symptoms
Look like a loss of normal functions, such as flattened affect and social withdrawal.
Cognitive Symptoms
Affect thinking, memory, and attention, impacting work and school performance.
Why Understanding Symptoms Matters
Recognizing these symptom categories helps in early detection, proper treatment planning, and better outcomes. Each category requires different management strategies.
Key Takeaways
- Schizophrenia typically appears in early adulthood and affects thinking, feeling, and behavior.
- Positive symptoms (hallucinations, delusions) and negative symptoms (flattened affect, social withdrawal) require different management strategies.
- Genetic risk, dopamine dysregulation, and early life stress are the main contributors.
- Antipsychotic medication combined with psychosocial therapies offers the best long‑term outcomes.
- Early detection and consistent support can dramatically improve quality of life.
Imagine hearing voices that no one else hears or believing that strangers are plotting against you. For many, those experiences are a daily reality, not a Hollywood plot twist. Schizophrenia is a chronic mental health condition that disrupts perception, thoughts, and emotions. While the name often triggers fear, understanding the why and how can turn confusion into actionable steps.
What Exactly Is Schizophrenia?
Schizophrenia is classified under the broader umbrella of psychotic disorders. It usually emerges between ages 16 and 30, though a small percentage develop symptoms later. The disorder is not a singular disease but a spectrum of experiences, ranging from mild reality testing issues to full‑blown psychosis. Worldwide, about 1 in 100 people will be diagnosed at some point, making it a significant public‑health concern.
Core Symptoms to Watch For
The Symptoms of schizophrenia fall into three categories: positive, negative, and cognitive. Recognizing them early can speed up treatment and reduce the impact on daily life.
- Positive symptoms: Hallucinations (most often auditory), delusions, disorganized speech, and erratic behavior. These add experiences that aren’t actually present.
- Negative symptoms: Flattened affect, reduced speech (alogia), lack of motivation (avolition), and social withdrawal. They look like a loss of normal functions.
- Cognitive symptoms: Trouble focusing, memory gaps, and difficulty planning. These often affect work or school performance more than the dramatic hallucinations.
Because the symptom mix varies, every treatment plan must be customized. A teenager with predominant hallucinations might need a different approach than an adult whose main challenge is social isolation.
Why Does It Happen? Causes and Risk Factors
There is no single cause; rather, schizophrenia results from an intricate web of Causes that include genetic, neurobiological, and environmental components.
Genetic Risk Factors
Having a first‑degree relative with schizophrenia raises your risk to about 10%-far higher than the 1% baseline. Researchers label specific DNA variations as Genetic risk factors such as copy‑number variations on chromosomes 1, 6, and 22. These aren’t destiny, but they set the stage for other triggers.
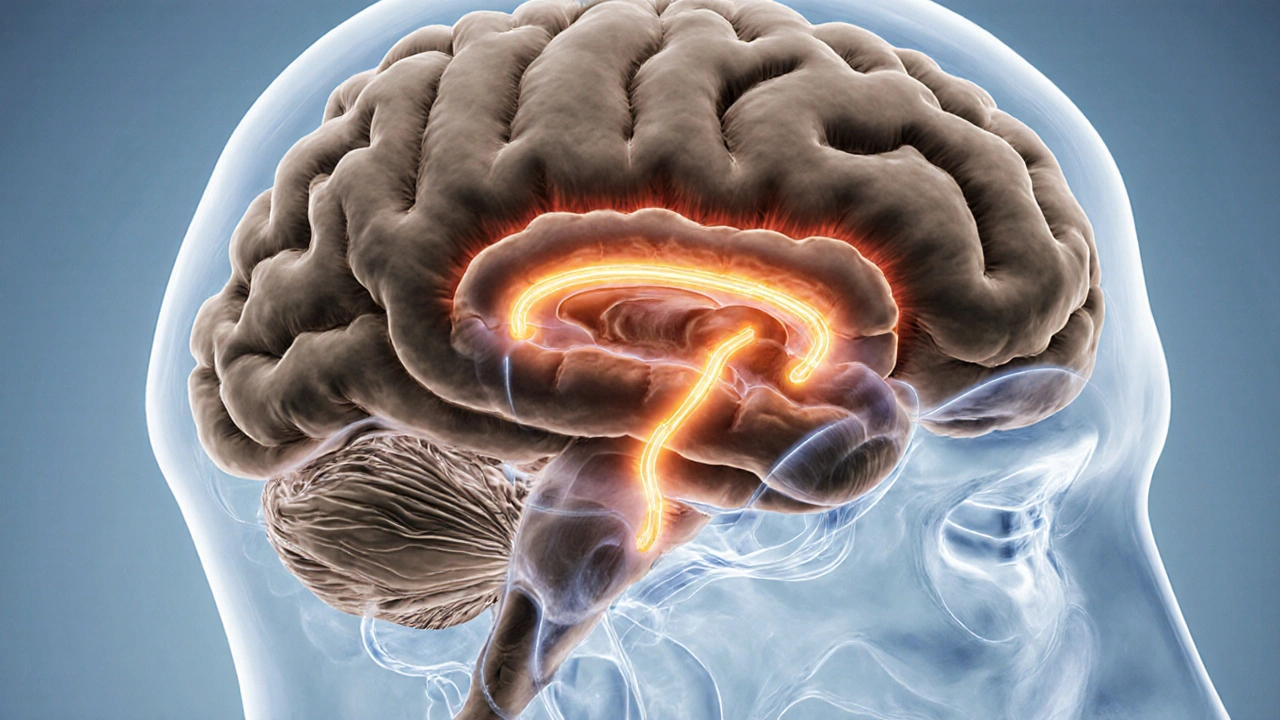
Brain Chemistry: The Dopamine Hypothesis
One of the most robust neurochemical models is the Dopamine hypothesis which suggests that excess dopamine activity in certain brain pathways leads to positive symptoms. Modern imaging shows over‑activity in the mesolimbic tract, while under‑activity in the prefrontal cortex relates to cognitive deficits.
Structural Brain Changes
Neuroimaging studies consistently reveal reduced gray matter volume in the frontal lobes and enlarged ventricles. These findings, captured through Neuroimaging techniques such as MRI and PET scans, help clinicians confirm diagnosis and monitor progression.
Environmental Influences
Early childhood adversity-trauma, neglect, or severe infection-interacts with genetic susceptibility. Cannabis use during adolescence, especially high‑THC strains, also doubles the risk of developing psychosis later.
How Is Schizophrenia Diagnosed?
There is no blood test; diagnosis relies on clinical interview, symptom duration (at least six months), and functional impairment. The DSM‑5 and ICD‑11 provide criteria, but many clinicians also use the Structured Clinical Interview for DSM (SCID) to ensure reliability. Early detection programs, like the Australian “Early Psychosis Intervention” network, run screening tools in schools and primary‑care clinics to catch prodromal signs before full psychosis emerges.
Treatment Options: A Holistic View
The most effective approach blends medication with psychosocial support. Below is a quick snapshot of what each pillar offers.
| Aspect | Antipsychotic Medication | Psychotherapy (e.g., CBT) |
|---|---|---|
| Primary Target | Positive symptoms (hallucinations, delusions) | Negative & cognitive symptoms, coping skills |
| Onset of Benefit | 1-2 weeks for acute relief | 4-6 weeks for measurable change |
| Side‑Effect Profile | Weight gain, metabolic syndrome, EPS | Low; occasional emotional discomfort |
| Long‑Term Outcomes | Reduced relapse when adhered to | Improved social functioning, reduced stigma |
Antipsychotic Medication
First‑line treatment involves Antipsychotic medication which blocks dopamine D2 receptors, thereby tempering the over‑active pathways linked to psychosis. There are two families:
- Typical (first‑generation) - Haloperidol, chlorpromazine. Stronger EPS (extrapyramidal symptoms) risk.
- Atypical (second‑generation) - Risperidone, olanzapine, aripiprazole. Lower EPS but higher metabolic side‑effects.
Choosing the right drug hinges on symptom profile, previous response, and health history. Clozapine remains the gold standard for treatment‑resistant cases, yet requires weekly blood monitoring due to rare agranulocytosis risk.
Adherence Tips
Non‑adherence drives relapse rates up to 80%. Strategies that work include long‑acting injectable (LAI) formulations, blister packs, and mobile reminder apps. Involving family members in medication planning also boosts consistency.
Cognitive Behavioral Therapy (CBT) and Other Psychosocial Interventions
Cognitive Behavioral Therapy for schizophrenia focuses on challenging delusional beliefs, reducing distress from hallucinations, and building coping skills. Sessions typically run weekly for 12‑20 weeks, with homework that reinforces reality testing.
Other effective therapies include:
- Family Psychoeducation - teaches relatives how to support medication adherence and de‑escalate crises.
- Social Skills Training - role‑playing daily interactions, improving employment prospects.
- Supported Employment Programs - provide job coaching and workplace accommodations.
Evidence shows that patients receiving CBT plus medication experience a 30% greater reduction in psychotic symptoms than medication alone.

Why Early Intervention Matters
The first few years after onset are critical. Studies from the Australian “First‑Episode Psychosis” cohort reveal that a 6‑month reduction in untreated psychosis correlates with a 15% improvement in functional outcomes at five years. Early intervention teams combine rapid assessment, low‑dose antipsychotics, and intensive psychosocial support to shorten the duration of untreated illness.
Living Day‑to‑Day with Schizophrenia
Beyond clinical care, everyday strategies can make a huge difference.
- Routine: Regular sleep, meals, and exercise stabilize dopamine cycles.
- Stress Management: Mindfulness, yoga, or simple breathing exercises lower cortisol, which can exacerbate psychosis.
- Substance Avoidance: Alcohol and recreational drugs, especially cannabis, can trigger relapse.
- Peer Support: Joining groups like the National Alliance on Mental Illness (NAMI) provides validation and practical tips.
While the diagnosis is lifelong, many people lead fulfilling careers, maintain relationships, and contribute creatively once the right treatment mix is in place.
Frequently Asked Questions
Can schizophrenia be cured?
There is no cure, but symptoms can be managed effectively with medication and therapy. Many individuals achieve remission and live independently.
How long does it take for antipsychotics to work?
Most patients notice a reduction in acute hallucinations within 1‑2 weeks, but full stabilization may take 4‑6 weeks.
Is cannabis linked to schizophrenia?
Heavy, high‑THC cannabis use during teenage years roughly doubles the risk of developing psychosis, especially in genetically vulnerable individuals.
What are long‑acting injectables and who should consider them?
Long‑acting injectables (LAIs) deliver a steady dose of antipsychotic over weeks or months, reducing daily pill burden. They suit patients with adherence challenges or frequent relapses.
Can lifestyle changes affect symptoms?
Yes. Regular exercise, balanced nutrition, adequate sleep, and stress‑reduction techniques can lower symptom severity and improve overall wellbeing.
Understanding schizophrenia isn’t about accepting a permanent limitation; it’s about navigating a complex condition with the right knowledge, tools, and support. With early detection, a tailored mix of medication and therapy, and everyday coping strategies, many people turn a daunting diagnosis into a manageable part of their lives.



Sebastian Miles
Great rundown-dopamine dysregulation, gray‑matter loss, and early‑intervention windows are all crystal clear.