Eye Pressure & Sleep Position Calculator
Quick Take
- Eye pressure (intraocular pressure) naturally fluctuates during the night.
- Both sleep position and sleep‑related disorders can raise or lower that pressure.
- Higher nighttime pressure is linked to a higher risk of glaucoma.
- Improving sleep hygiene and treating apnea can help keep eye pressure stable.
- Regular eye exams are essential if you have risk factors.
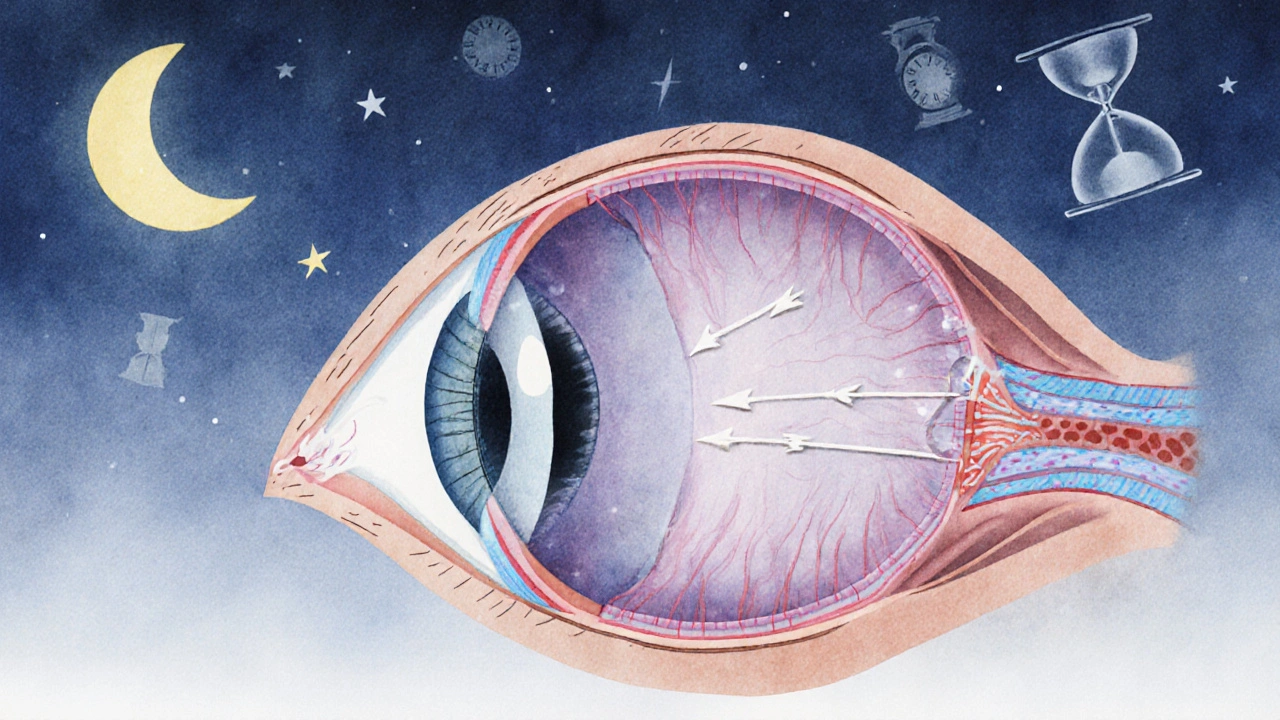
Eye pressure is a measurement of the fluid (aqueous humor) that fills the front part of the eye, expressed in millimeters of mercury (mmHg). Maintaining a healthy range-typically 10 to 21mmHg-is crucial because prolonged elevations can damage the optic nerve and lead to glaucoma.
eye pressure doesn’t stay constant; it follows a daily rhythm that’s surprisingly tied to how we sleep.
What Controls Eye Pressure?
The eye constantly produces and drains a clear fluid called aqueous humor. Production happens in the ciliary body, while drainage occurs mainly through a spongy tissue called the trabecular meshwork. When production outpaces drainage, pressure climbs.
Key players in this balance include:
- The optic nerve, which is sensitive to pressure spikes.
- blood pressure, which can affect fluid dynamics in the eye.
- The body's circadian rhythm, a 24‑hour internal clock that regulates hormone release and fluid movement.
How Sleep Affects Eye Pressure
Research from the American Academy of Ophthalmology shows that intraocular pressure (IOP) tends to rise during the night, peaking in the early morning hours. Three main mechanisms drive this pattern:
- Body position: Lying flat reduces the eye’s drainage angle, especially when you sleep on your stomach or side. Studies of 200 volunteers found a 2‑3mmHg increase in IOP when participants slept prone versus supine.
- REM sleep: Rapid‑eye‑movement sleep is associated with higher sympathetic activity, which can temporarily boost both blood pressure and IOP.
- Fluid redistribution: While you’re recumbent, blood and interstitial fluids shift toward the head, raising the volume of aqueous humor.
For most people, these fluctuations stay within a safe range. But if you already have borderline pressure or a family history of glaucoma, nightly spikes matter.
Sleep Disorders that Influence Eye Pressure
Conditions that disturb normal sleep architecture can amplify IOP changes:
- Sleep apnea-characterized by intermittent breathing pauses-causes repeated oxygen drops. A 2023 meta‑analysis of 12 studies linked moderate‑to‑severe apnea with an average nighttime IOP increase of 1.8mmHg.
- Chronic insomnia often leads to fragmented REM cycles, which can keep sympathetic tone elevated and prevent the natural nocturnal dip in pressure.
- Restless‑leg syndrome and periodic limb movements raise systemic inflammation, indirectly affecting the trabecular meshwork’s ability to clear fluid.
If you’ve been diagnosed with any of these disorders, it’s worth asking your ophthalmologist to monitor IOP more closely.
Practical Ways to Keep Nighttime Eye Pressure in Check
Below are evidence‑backed habits that help smooth out the pressure curve:
- Sleep on your back. A simple pillow‑prop technique that keeps your head slightly elevated (10‑15cm) can lower IOP by up to 1mmHg compared with stomach sleeping.
- Maintain a consistent schedule. Going to bed and waking up at the same time each day stabilizes circadian rhythms, which in turn moderates hormone‑driven fluid shifts.
- Treat apnea early. CPAP therapy has been shown to reduce nighttime IOP spikes by 1‑2mmHg in randomized trials.
- Limit caffeine after noon. Caffeine can raise both blood pressure and IOP for up to six hours; cutting back in the afternoon helps the evening dip.
- Stay hydrated, but avoid excess fluid before bed. Drinking large amounts right before sleep can temporarily increase aqueous humor production.
When to Seek Professional Help
If you notice any of the following, schedule an eye exam promptly:
- Family history of glaucoma or personal diagnosis of ocular hypertension.
- Repeated headaches that feel worse in the morning.
- Visual disturbances such as halos around lights or peripheral loss.
- Diagnosed sleep disorder that’s poorly controlled.
During the exam, the doctor will use tonometry to measure IOP at different times of day. Some specialists even conduct overnight monitoring to capture the true pressure pattern.
Comparison of Eye Pressure Changes by Sleep Position
| Sleep Position | Average IOP Change (mmHg) | Risk Level for Glaucoma Progression |
|---|---|---|
| Supine (back) | +0.5 to +1.0 | Low |
| Lateral (side) | +1.0 to +2.0 | Moderate |
| Prone (stomach) | +2.0 to +3.5 | High |
These numbers are averages; individual responses can vary based on age, baseline pressure, and underlying eye anatomy.
Bottom Line
Sleep isn’t just rest for the brain-it’s a key regulator of the fluid pressure inside our eyes. By tweaking sleeping habits, treating apnea, and staying vigilant with eye exams, you can keep eye pressure from creeping into dangerous territory.
Frequently Asked Questions
Does sleeping on my side increase my risk of glaucoma?
Side‑sleeping can raise intraocular pressure by about 1‑2mmHg compared with back‑sleeping. For most people the increase is harmless, but if you already have high pressure or a family history of glaucoma, it’s wise to favor a supine position.
Can CPAP therapy lower my eye pressure?
Yes. Studies show that consistent CPAP use can reduce nighttime IOP spikes by 1‑2mmHg, likely by stabilizing oxygen levels and reducing sympathetic surges.
Why does my eye pressure feel higher in the morning?
During sleep, fluid accumulates in the head and the eye’s drainage angle can be compressed. This leads to a natural early‑morning rise, which is why many eye‑pressure measurements are taken later in the day for consistency.
Should I drink water before bedtime?
Staying hydrated is important, but large volumes right before sleep can temporarily boost aqueous humor production. Aim to finish most of your fluid intake at least an hour before bedtime.
Is there a link between caffeine and eye pressure?
Caffeine can cause a short‑term rise in both blood pressure and intraocular pressure lasting up to six hours. Cutting back after noon helps maintain a smoother nighttime pressure dip.



Anupama Pasricha
I appreciate the way the article breaks down the physiology behind intraocular pressure. It’s not often that you see a clear link between sleep position and fluid dynamics in the eye. For anyone dealing with borderline IOP, even a small habit change like backing off the stomach‑sleeping could matter. Keep the practical tips coming!